Human Embryonic Stem Cells: Science, Ethics & Future Use

Perspectives from the IVF Lab
Written by Prof. Dr. Darren Griffin and Guy Griffin
Research Professor: University College London, University of Kent, Royal Veterinary College London & Undergraduate in Biochemistry, University of Southampton
The world of IVF (in-vitro fertilization) and genetics is largely concerned with the diagnosis of genetic disease in human embryos. In general terms, we investigate and implement new ways in which we can diagnose disease. We debate whether we should sequence whole genomes, whether we are accused of “playing god” through “designer babies” and whether we should manipulate the genes of human embryos. An area that touches upon our consciousness from time to time however it that of human embryonic stem cells (hESCs).
Table of Content
What are Stem Cells?
Stem cells are undifferentiated, and the point of them in research and medicine is that they have the great potential to become many types of specialised cell.
We hear a lot of terms used to describe them including “totipotent” – this means the ability to turn into any sort of cell type in the human body, including the placenta; “pluripotent” which means the ability to turn into most types of human cells or “multipotent” – the ability to turn into a reasonably large number of types.
Each of these terms denotes, by definition, a more restricted range and usefulness, but “totipotent and pluripotent”, as well as “pluripotent and multipotent” are sometimes used interchangeably.
Human IVF embryos are essentially a ball of human embryonic stem cells (hESCs) and their ability to differentiate into any cell type is what fuels their interest for revolutionary treatments and in fundamental scientific research.
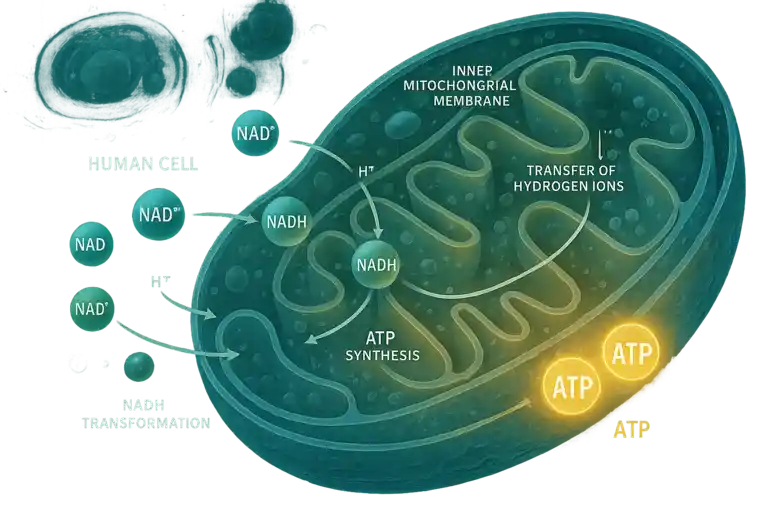
Stem cells, distinct from other cell types in the body, possess two key qualities:
the ability to self-renew indefinitely (for most types) and the capacity to differentiate into specialized cells.
Based on their origin and differentiation potential, stem cells can be classified into two main categories:
embryonic stem cells and adult stem cells.
Adult stem cells can be induced into pluripotency (induced pluripotent stem cells – iPSCs) but that is a whole different area that is not considered here. Moreover, new techniques of cellular reprogramming that have been adapted for the process of transdifferentiation, the ability of cells to switch from one specialized cell type to another directly, sometimes without reversal into a less specialized cell are not considered here.
Rather, we will only deal with cells that are directly derived from human IVF embryos; in practical terms, this means cells generated thanks to the generosity of IVF patients donating their embryos for research, despite their initial motivation being to try and find a solution to their own infertility or their risk of transmitting genetic disease.
As a result of the efforts of these unselfish individuals, stem cells have become pivotal in the fields of regenerative medicine and biomedical research. It is the very uniqueness of their properties that raise the most pertinent ethical issues.
That is, each embryo is potentially a human life and thus worthy of the dignity and respect that such a status demands. IVF embryos and the stem cells derived from them are undoubtedly extraordinarily valuable for research and potential therapies, but the balance between their potential benefit and the understandable ethical concerns that their use raises is a delicate one. The only certainty is that not everyone will agree.
Obtaining Human Embryonic Stem Cells (hESCs)
All hESCs start life in the IVF clinic.
Human eggs are harvested by ultrasound-guided aspiration from the ovary.
Once they are exposed to, or injected with sperm, a proportion develop into a one cell zygote with a unique genetic constitution. One cell becomes two, two become four, four become eight and, within days, a small ball called a “morula” (the same term is used for a raspberry or blackberry fruit) forms.
The first stage of differentiation occurs at around day five post-fertilization when about half the embryos form an “inner cell mass” – this is exactly as its name suggests, a ball of cells in the middle. It is surrounded by a hollow ball of cells called the trophectoderm, and the rest of the “void” is occupied by a fluid-filled cavity called the blastocoel. The inner cell mass might, if implanted, become a baby and the trophectoderm would become the placenta.
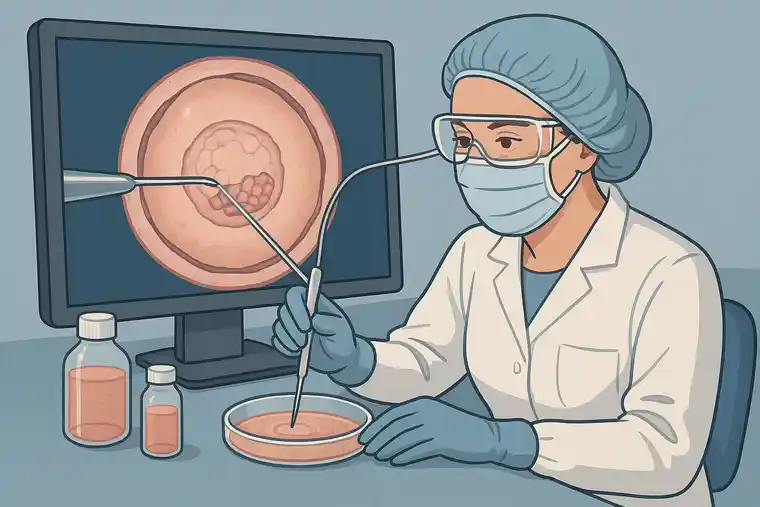
hESCs are isolated by an experienced embryologist, micromanipulating out the inner cell mass and placing it into a culture dish.
From there, cell biologists take over and, using their knowledge of developmental processes, send the cells down pathways of differentiation appropriate to their specific applications. hESCs typically grow in compact colonies on feeder layers of fibroblasts, which produce the extracellular matrix for cell attachment and condition the culture medium with paracrine factors.
Protein substrates (e.g. matrigel, laminin, vitronectin) and synthetic matrices can also be used for cell derivation and/or culture. hESCs can proliferate indefinitely, while still preserving their pluripotent characteristics. This combination of IVF and molecular cell biology has opened-up insight into the worlds of human development, disease modelling and drug testing:
Potential Applications of hESCs
The applications of hESCl technology are broad:
- In regenerative medicine hESCs hold the promise for regenerating damaged tissues and organs. For instance, they can be differentiated into cardiovascular cells to treat heart disease or neural cells to repair spinal injuries.
- In disease modelling and drug testing, cell biologists use hESCs to create specific cell types that mimic diseases. For example, hESC-derived cardiomyocytes are used to study conditions such as cardiac arrhythmias and test drug safety and efficacy.
- In the field of gene therapy, hESCs can be genetically modified to correct mutations associated with genetic disorders, providing a potential cure for conditions like cystic fibrosis or muscular dystrophy.
- In the world of organ transplantation, the ability to create organs or tissues from hESCs could address the donor organ shortage, reducing waiting times and rejection rates associated with transplants.
- In cancer research, hESCs can help in understanding cancer biology by enabling researchers to study the earliest stages of tumour formation thus identifying new therapeutic drug targets.
It is therefore very clear that a large part of the future of medicine lies in hESC research, offering treatment possibilities for a wide range of diseases in tandem with the body’s own healing mechanisms. It will provide fundamental insight, but the field faces many ethical dilemmas, posing an argument between morality and furthering scientific innovation.
Ethical Concerns
The IVF world is no stranger to ethical dilemmas: When Bob Edwards and Patrick Steptoe produced the world’s first IVF baby Louise Brown, there was outrage in many quarters.
When the Munday twins first appeared as a result of Alan Handyside’s efforts in preimplantation genetic diagnosis, we were accused of “playing God” and producing “designer babies.”
The concept of saviour siblings spawned films like “My Sister’s Keeper” and now the ability to sequence whole embryonic genomes or edit the genes of IVF embryos brings new ethical challenges.
The ethical problems lie in the fact that the totipotent inner cell mass can be seen, in the eyes of some, as a potential or current human life. The creator of the first isolated embryonic stem cells, James Thompson, once said “If human embryonic stem cell research does not make you at least a little bit uncomfortable, you have not thought about it enough”.
It is for this reason, we decided to write this as a father-son combination. We each share 50% of each other’s genomes, varying proportions of which were present in our forefathers and will, with luck, be in our descendants.
While neither of us are products of IVF, we were both once embryos with inner cell masses – our cells could have had a very different fate as the subject of hESC research.
Various arguments are proposed as to what makes a human life significant: its potential, its viability, its consciousness, its sentience. Such terminology inevitably introduces controversy into the argument, as there is no scientific answer to these questions.
Is there a defined age when consciousness emerges?
For instance, the earliest memory of a close friend is folding origami in a dress aged four. No right-minded person would seriously suggest that a four-year-old is not worthy of the dignity of life because of their absence of consciousness (if this is true), but the question of how early in development we should consider an embryo or fetus to be a sentient being is an intriguing one.
Current legislation in many countries allow, with parental consent, ethically justified use of “spare” embryos for hESCs research.
Contrast this, if you will, with the case of Julius Hallervorden – a Nazi scientist who is credited with making discoveries that furthered our understanding of cerebral palsy and many types of brain cancer but did this by using the brains of already dead eugenics victims (that would have otherwise been buried or cremated).
Was he wrong to take this opportunity to research the brain?
Did he have a moral responsibility to use these samples (or indeed not to use them) with the prospect of saving more lives in the future?
The field of surgery was, it is claimed, significantly furthered by the questionable practices of Burke and Hare by digging up the graveyards in Edinburgh. Lives were inevitably saved but the dignity of human life was nonetheless impinged.
Aristotle’s ethics as virtue claims that morality is based on purpose i.e. a good soldier is one that performs their duties well. Would this make Hallervorden a ‘good scientist’ and thus his actions morally right?
On the other hand, if we take the view of Kantian deontology, we can claim that he ignored his duty as a physician to first preserve human life (the guiding principle of the Hippocratic oath is “first do no harm”) in the pursuit of tools for research?
Essentially, the ethical framwork for and against hECSs is built around the following:
- The embryo’s moral status: hESC opponents argue that human life begins at conception, thereby equating the use of an embryo for hESCs to murder. This is a viewpoint supported by some religious beliefs and philosophical perspectives.
- Utilitarian perspective: hESC proponents argue that the potential benefits of hESCs, alleviating suffering and advancing scientific knowledge often outweigh the ethical concerns.
- Regulation and guidelines: Ethical oversight is crucial in hESC research, but countries vary greatly in their guidelines, this could present worldwide issues.
- Alternatives exist: iPSCs potentially provide a solution that alleviates some of the ethical concerns.
The questions over hESCs won’t go away any time soon however as they will play a huge role comparisons to iPSCs in order to test their efficacy. iPSCs continue to be hugely useful but few would pretend that they are, yet, as useful as hSECs for all applications.
The ethical question of the use of hESCs is a therefore deep well of ethics with no correct answer. Even with the increasing use of iPSCs, hESCs are likely to be with us for some time.
Technical concerns
hESCs are ultimately intrinsic parts of developmental biology. Being able to use them effectively however depends on truly understanding how they develop and the processes they go through. Despite their vast potential therefore, they still have several challenges currently hindering their widespread application:
Immune rejection: the body may recognize hESCs as foreign.
Tumorigenicity: There is a risk that transplanted stem cells could form tumours, as their uncontrolled proliferation may lead to the development of teratomas.
Standardization and QC: For hESC-derived therapies to be effective, it is crucial to establish standardized processes for cell culture, differentiation, and testing. Variability in these processes would lead to inconsistent results in clinical applications.
Public perception and funding: Ongoing debates surrounding the ethical implications of hESC research certainly can slow funding opportunities and public support.
We, as scientists in both the established and the future generation must thus continue to engage with the public, providing education about the potential benefits and ethical guidelines that govern research, particularly pertaining to hESCs.
Blastoids: More innovation from the IVF lab

Blastoids are synthetic constructs resembling human IVF blastocysts; they are emerging as a significant tool in hESC research as, like iPSCs, they circumvent some of the ethical issues surrounding hESC use.
Blastiods more closely resemble hESCs than iPSCs; that is, they contain important signalling pathways that drive cell differentiation and mimic key properties of natural blastocysts such as inner cell mass and trophectoderm-like compartments.
Blastoids exhibit essential features that are crucial for understanding how embryonic stem cells develop, for instance, in investigating the dynamics of cell-cell interactions and the establishment of cell lineages. Blastoids are not however usually considered as embryos themselves and thus blastoid research sidesteps many of the ethical concerns associated with hESCs.
As with hESCs, however, blastoid research not only enhances our grasp of developmental biology but also holds great potential for innovative applications in regenerative medicine, drug discovery and modelling congenital diseases.
Through precise manipulation of the conditions under which blastoids are formed, scientists can tailor differentiating pathways, facilitating studies on various developmental disorders and diseases. Blastoids serve as a platform for testing therapies for conditions affecting early embryonic development.
For example, if researchers wish to examine the impact of specific genetic mutations linked to congenital disorders, they can introduce these mutations into the initial stages of blastoid development and analyze resultant phenotypes.
This capacity extends the potential of blastoids as a viable model for understanding various diseases, leading to breakthroughs in targeted therapies.
Another promising application of blastoids involves the field of regenerative medicine. With the ability to generate different cell types; blastoids can potentially aid in crafting organoids or even organ tissue for transplantation.
Through targeted differentiation, researchers could guide blastoids to develop specific tissues, offering new pathways for regenerative strategies that could repair damaged organs or treat degenerative diseases.
Blastoids also provide a novel approach in the preliminary stages of drug discovery. Researchers can use these constructs to test drug responses in cellular environments that closely resemble early developmental stages, paving the way for identifying drugs that may impact stem cell behaviour and differentiation.
This leads to improved utility in pharmaceuticals, as researchers can discover which compounds effectively promote or inhibit certain pathways within human cells.
Blastoids thus represent a groundbreaking tool in human embryonic stem cell research.
Their ethical advantages, combined with their hESC-like abilities could, in fact, revolutionize how we approach developmental biology and therapeutic interventions.
The Future of hESC Research
hESCs (and, to some extent, blastoids) hold immense promise that, as scientists, we are only beginning to exploit.
Coupled with editing and improved tissue-engineering techniques, hESCs have great potential for:
- Personalized medicine: patient-specific stem cell lines that address unique genetic profiles, allowing for tailored therapies that minimize rejection and enhance effectiveness.
- Collaborative international research: Global collaborations expediting research and standardization processes, facilitating the sharing of knowledge and techniques that can lead to more rapid advances in the field.
- Integration with other technologies: Combining hESC research with other emerging technologies, such as artificial intelligence and bioinformatics, could revolutionize the way clinicians and scientists approach diseases and treatment protocols.
- Continued ethical dialogue: Ongoing discussions about the ethical considerations surrounding hESC use will be crucial alongside public engagement and transparent discourse. Only through this can we navigate the complexities involved in the ethical implications of stem cell research.
Conclusion
Human embryonic stem cells (hESCs) stand out as one of the most intriguing and contentious fields in contemporary biomedical research. Their capacity to transform medicine through regenerative treatments, disease modelling and drug testing is undeniable.
However, these enormously promising prospects must be weighed against the profound ethical dilemmas concerning the moral status of embryos.
As research advances, the emergence of alternative stem cell sources, iPSCs, transdifferentiation and blastoids, will inevitably mitigate certain ethical concerns while providing similar advantages. Despite this, these are unlikely to be a “cure all” and hESCs will continue to be a critical focus of investigation, prompting ongoing dialogue among scientists, ethicists and the public regarding the future of this technology and its societal implications.
Grasping and addressing these complexities will help define the direction of medical practice, with the potential to affect millions of individuals through groundbreaking therapies and enhanced understanding of human biology.
The field of hESC research started in the IVF lab and remains dynamic to this day. Its evolution will undoubtedly shape the course of medical science in professors, undergraduates and further generations to come.
MedClinics offers quality stem cell treatment in Istanbul, Turkey at affordable prices! Please contact us now for a detailed consultation!
Stay Updated
Follow our blog for the latest in medical and aesthetic treatments, tips for maintaining healthy teeth, and inspiring patient success stories.
Short Biographie Prof. Dr. Darren Griffen
Darren Griffin is a Professor of Genetics at the University of Kent, specializing in cytogenetics and reproductive genetics. His research focuses on chromosome biology, fertility, and preimplantation genetic diagnosis. A prominent figure in his field, Professor Griffin has authored numerous scientific publications and is actively involved in science communication and education. He is also associated with UniversityTech.io, contributing to advancements at the intersection of genetics and technology.