Exosome Therapy for Autism in Istanbul, Turkey: A New Path in Regenerative Neuroscience – Insights by Prof. Dr. Erdinç Civelek, MD, PhD (C)
A New Conversation About Exosome Therapy for Autism – and the Smallest Messengers We Know
Written by Prof. Dr. Erdinç Civelek, MD, PhD (C)
As a physician, I’ve sat across from many parents who’ve just heard the word “autism” for the first time. It’s rarely a moment they forget. There’s confusion, fear, often guilt, and always love – an overwhelming desire to do something, anything, that might help their child connect a little more with the world.
We’ve come a long way in how we understand autism spectrum disorder (ASD). It’s not a disease. And it’s not a character flaw. But when a child screams through the night, avoids all eye contact, or spends hours rocking back and forth – those things aren’t just “quirks.” They can be painful, for the child and the family. I’ve seen mothers cry because their child hasn’t spoken in years. Fathers who quietly ask if they did something wrong. They didn’t. But they need options. Real ones.
Sometimes I get asked, “Do you think this can cure autism?” And I always pause. Because that’s not the right question. Autism isn’t something broken. But there are children who hardly speak, who can’t sleep, who bang their heads on the wall out of frustration. Parents who haven’t heard their child call them “mama” or “baba” in years. These are the cases where I look deeper, medically. Not to fix the child – but to ease what hurts, to help them find their own version of calm, of clarity.
In some of these children, we see signs of chronic neuroinflammation in the brain. Not always – but often enough to matter. And when we calm that inflammation – whether by diet, oxygen, stem cells, or now, exosomes – things begin to shift. Sometimes slowly. Sometimes surprisingly fast.
Exosomes aren’t magic. But they are real, biological, and – here’s the key – they don’t need to be cells to make a difference. They are cargo compounds and carry signals. Tiny messages between tissues. And in some children, those signals seem to help the brain settle. That’s what we’re beginning to understand. Not theory -observations. Experience.
In the next section, I’ll explain what exosomes actually are – without the fluff. Just enough to see why they matter.
Table of Contents
Understanding Exosomes: What They Are and Why They Matter in the Brain
If you haven’t heard of exosomes before, you’re not alone. Even many doctors are just starting to pay attention to them. For a long time, they were thought to be useless – just little bubbles that cells released to get rid of waste. We now know that assumption was wrong. Very wrong.
Exosomes are tiny vesicles, far smaller than a cell – more like a whisper in comparison. But inside that whisper is a message. They’re filled with molecules: proteins, some important groth factors, microRNAs, messenger (m) RNA’s, lipids, sometimes even fragments of mRNA. All of it packed into a nanosized envelope, sealed by a membrane, and sent from one cell to another.
The body uses these vesicles constantly. One cell “talks” to another by sending out exosomes. It’s not random. It’s deliberate. Think of them like carefully written notes passed between classmates in a very complex school – only the notes are made of bioactive signals, and the school is your nervous system, immune system, gut, and every organ in between.
Most of the exosomes we work with in therapy today come from mesenchymal stem cells (MSCs). Not because they’re magical, but because they’re smart. These cells are known for their anti-inflammatory and regenerative properties. Their exosomes carry similar traits—but without the complexities and possible risks of using live cells.
Here’s what makes exosomes truly fascinating in the context of autism:
They’re small enough to cross the blood-brain barrier. That’s a major hurdle for most therapies targeting the brain. But exosomes? They slip through. Quietly. Effectively.
Even more interesting, they can be delivered in a way that makes sense for the child – intravenously, intranasally and intrathecally. And they don’t stay strangers to the body. Because they’re not synthetic. They’re natural. Biologically familiar.
So no, they’re not science fiction. They’re not fantasy. They’re part of a language the body already understands. We’re just learning how to listen – and how to speak it back.
Why Exosomes Are Relevant for Autism
Every child with autism is different. That’s not a slogan – it’s a clinical reality. Some children speak early but struggle with social cues. Others don’t speak at all. Some flap their hands, line up toys, or spin for hours. Others have explosive meltdowns triggered by light, sound, or even a texture on their skin.
For a long time, we’ve treated autism as a purely neurological condition – something happening in the wiring of the brain. And that’s still true. But it’s not the whole story.
In the past decade, a growing number of studies have pointed toward a biological component beneath the surface:
- Chronic neuroinflammation
- Disrupted immune signaling
- Imbalanced microglia activity (the brain’s immune cells)
- Altered gut-brain communication
In simpler terms: for some children on the spectrum, their brains are not just wired differently – they may also be inflamed, overwhelmed, or misfiring in how cells talk to one another.
This is where exosomes become incredibly relevant.
They don’t just “do something.” They modulate. They carry molecules that can turn down overactive immune responses, calm inflammation, and encourage a more stable internal environment -especially inside the brain. It’s not suppression. It’s regulation.
Let me give you a clinical image. Imagine a child whose nervous system is constantly in a fight-or-flight state. Noise is louder. Light is sharper. The world feels unsafe. Now imagine tiny messengers entering the brain and gently nudging those overactive immune cells to stand down. Less cortisol. Less cytokine noise. More room for focus, for connection, maybe even for speech.
Of course, this doesn’t happen in every child. And it doesn’t happen overnight. But in the right cases – with the right medical indications – I’ve seen changes that are hard to ignore.
In truth, we don’t need exosomes to “fix autism.” But if they can help reduce the internal storm – the neuroinflammatory chaos that some children live with – then that’s already a gift. A real, biological intervention with observable effects.
And that’s why we’re looking at them so closely.
Scientific Foundation: What Current Studies Show about Exosome Therapy for Autism
When parents hear “exosomes,” they often ask the most important question first: “Is this actually studied? Or just experimental?” And they’re right to ask. It’s our job as doctors not to offer hype – but to offer truth, even when the data is still young.
So here’s the truth:
Yes, exosomes have been studied in the context of autism. And the results are cautiously optimistic.
Exosomes – especially those derived from stem cells – have been studied in both animal models and early human trials related to autism. The overall findings are cautiously positive. Researchers have observed improvements in social behavior, communication, emotional regulation, and sleep. There’s also biological evidence that exosomes help reduce brain inflammation, balance the immune system, and support better neural connections.
Importantly, the therapy has generally been well tolerated, even in very sensitive individuals. While large-scale clinical trials are still ahead, the science so far aligns with what we’d expect based on how exosomes work in the body.
So yes – exosome therapy for autism is still evolving. But it’s not wild speculation anymore. It’s early science, grounded in real data, driven by genuine clinical need.
Mechanisms of Action: How Exosomes May Support Neurodevelopment
Understanding how exosomes might help in autism isn’t about believing in miracles. It’s about following the biology – step by step – until the picture makes sense.
So let’s take a quiet look under the microscope.
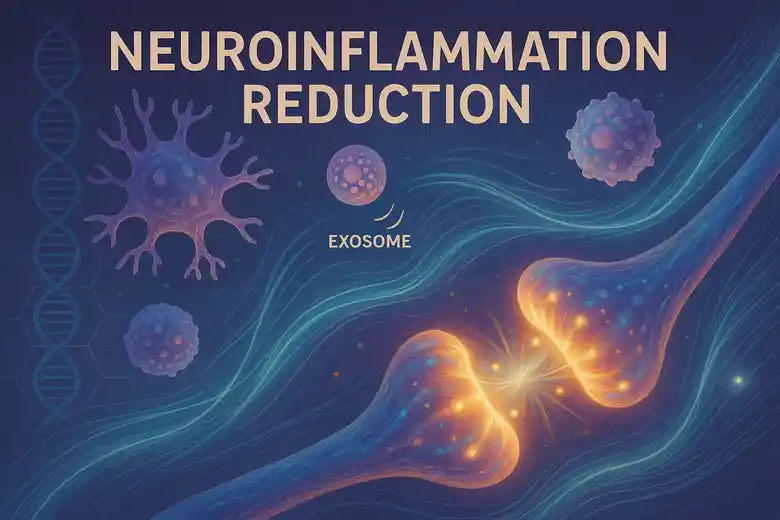
1. Reducing Neuroinflammation
Many children with autism show signs – either in lab markers, behavior, or MRI imaging – of chronic low-grade inflammation in the brain. This isn’t always visible, but it can disrupt the delicate balance of neural signaling, especially in early development.
Exosomes from mesenchymal stem cells carry anti-inflammatory molecules like:
- TGF-β1 (transforming growth factor)
- IL-10 (interleukin-10)
- small RNA fragments that downregulate pro-inflammatory pathways
When these vesicles reach the brain, they interact with microglia – the immune watchdogs of the CNS. Instead of triggering them, exosomes tend to nudge them toward a more regulatory, calming state. Less fire. Less noise. More space for development.
2. Supporting Synaptic Plasticity
The brain is not static. Especially in children, it’s constantly rewiring, pruning, adapting. Exosomes may support this process by:
- Carrying neurotrophic factors (like BDNF – brain-derived neurotrophic factor)
- Delivering microRNAs that regulate gene expression in neurons
- Helping neurons build and rebuild synapses, the connections where learning and communication happen
In children with ASD, we often see either excessive synaptic density or poorly regulated pruning. Exosomes might help restore a more natural balance – allowing the brain to fine-tune its own structure.
3. Balancing the Immune-Brain Dialogue
Autism isn’t just “in the head.” More and more evidence points to a two-way street between the immune system and the nervous system – and in some children, that conversation seems to be confused or overheated.
Exosomes can enter lymphoid tissues, interact with T cells, and modulate cytokine release in the gut-brain axis. Some researchers believe that’s part of why we sometimes see improvements not just in behavior, but in digestion, sleep, and general mood stability after treatment.
4. Crossing the Blood-Brain Barrier – Naturally
Unlike many therapies, exosomes don’t need help to reach the brain. Their small size (30–150 nm) and lipid bilayer structure allow them to cross the blood-brain barrier almost effortlessly – especially when administered intranasally, where they can reach the olfactory bulb and deeper brain regions directly via brain lymphatic system.
That’s not a side effect. It’s part of their design. Nature built them for communication – even across the most selective membranes in the body.
When you put all of this together, you don’t get a miracle cure. You get a biological tool that helps the brain remember how to regulate itself. A tool that listens before it speaks. One that doesn’t overwrite the system – but invites it to rebalance.
And for some children, that invitation seems to be exactly what their brain has been waiting for.
Clinical Applications: Dosing, Delivery, and Protocols in Exosome Therapy for Autism
Let’s move from theory to reality. What does exosome therapy actually look like in practice – when a real child walks into a real clinic?
First of all: this is not a one-size-fits-all protocol. Every child is different. Every brain is different. And that’s exactly why a proper medical evaluation must come first. No exceptions. We start with a detailed history, behavioral assessment, blood work, and – if available – neuroimaging and immunological markers. We don’t treat autism. We treat the child behind the diagnosis.
Dosage: Less Can Be More
Unlike traditional drugs, exosomes don’t work based on milligrams per kilogram. Their power lies in the information they carry, not in volume. We typically work with concentrations of 50 – 100 billion particles per dose.
Many children show measurable responses after just one or two sessions, but in most of the cases—especially with significant language delay or aggressive behavior – we recommend a protocol of three cycles, with a break of one week between them.
Delivery Methods: Meeting the Brain Where It Lives
There are several ways to deliver exosomes. Each has its own logic:
- Intranasal (IN):
This is the most direct, non-invasive method for brain access. Exosomes are absorbed through the nasal mucosa and enter the olfactory pathway – reaching areas like the limbic system and prefrontal cortex. Children tolerate this well, even those with sensory sensitivities. - Intravenous (IV):
Useful for systemic immune modulation and full-body signaling. IV also allows for broader biodistribution. - Intrathecal (IT):
This is a spinal injection. It delivers exosomes directly into the cerebrospinal fluid and is always performed under light sedation.
Frequency and Duration
This is not daily therapy. We mostly administer exosomes in all three ways with a break of 1 week between to get the best positive effect.
Often, families report changes within days. Sometimes within hours. Sometimes after a few months.
Combining With Other Modalities
In some cases, exosomes are used in combination with mesenchymal stem cell therapy (hybrid treatment). The cells provide a structural “kickstart,” while the exosomes help sustain communication between neural and immune cells.
Because the goal isn’t just neural change. It’s functional change—in daily life, in family dynamics, in how the child experiences the world.
In short, exosome therapy isn’t just about delivery. It’s about timing, dosage, listening, and trust. It’s not a protocol. It’s a relationship – between the biology, the clinician, and the child.
Case Insights and Real-World Observations
In medicine, we’re trained to value numbers. Lab values, imaging results, symptom scores. But in autism care, some of the most meaningful changes aren’t found on a chart. They show up in the quietest places – between the lines of a parent’s voice.
I’ll never forget one mother, whose 6-year-old son had been entirely nonverbal. We had done three rounds of exosome therapy intranasally, intravenous and intrathecal. Three weeks later, she called – not frantic, but stunned.
“He looked me in the eyes,” she said. “For the first time in years. And then he said, ‘car.’ That’s all – just one word. But it was him. I know it was him.”
Another child, 8 years old, used to scream and bang his head for hours. We weren’t even sure he’d tolerate the therapy. But he did. Slowly, week by week, the outbursts shortened. He began sleeping through the night. For the first time, he hugged his little sister without hitting her moments later. Not a miracle. But a door opened.
One of the more subtle cases came from a teenager – 14, deeply anxious, barely able to handle noise. After three cycles of exosomes, he told his therapist, “The world feels quieter.” That phrase stuck with me. We hadn’t changed the world. But we may have helped his nervous system interpret it differently.
Not every child responds. That’s important to say. And not every response is fast. Some changes are so small you almost miss them – until you realize they’re happening every day, like a faint melody getting louder.
Sometimes it’s improved gut function. Sometimes language begins to emerge. Sometimes it’s emotional regulation – less flinching, more curiosity, fewer meltdowns. And sometimes… there’s just a softness in the child’s face you hadn’t seen before.
None of this replaces therapy. It doesn’t erase autism. But in children where chronic neuroinflammation plays a role, exosomes may give the brain a little more room to breathe, to learn, to connect.
And when a parent says, “He’s calmer. He’s more here,” – you pay attention. You write that down.
Because that’s not placebo. That’s biology doing something quiet, and real.
Risks, Safety, and Regulatory Perspective
Let me start with the most important sentence in this entire article:
No biological therapy should ever be administered to a child without clear medical indication, qualified oversight, and ethical responsibility. That includes exosomes.
We are working with living systems here – not pharmaceuticals, not algorithms. The very strength of exosomes – their subtle, intelligent communication with cells – also makes them powerful in ways we don’t fully control.
So, what do we know about safety?
So far, the safety profile of exosomes – especially those derived from umbilical cord MSCs – is encouraging.
In both animal studies and human trials:
- No major adverse effects were observed
- No immune rejection has been reported (due to their acellular nature)
- No evidence of toxicity, tumorigenicity, or long-term organ damage
In clinical settings, what we usually see are mild, short-term effects, such as:
- Fatigue
- Temporary irritability
- Nasal congestion (after intranasal delivery)
These effects typically resolve within 24–48 hours without intervention.
What are the real concerns?
- Standardization:
Not all exosomes are equal. Purity, particle concentration, origin, and preparation methods vary widely. Clinics that cannot provide full quality control data, including sterility, endotoxin levels, and size profiling, should not be trusted. - Overuse:
Some parents, understandably desperate for improvement, may seek many multiple sessions too quickly. But more is not always better. The immune system – especially in children – needs space to integrate. - False promises:
Any clinic claiming guaranteed speech recovery, full behavioral normalization, or “permanent cure” is not practicing medicine. They’re selling hope, not science.
What about regulation?
Currently, exosomes are considered biological products, not drugs, in most countries. That puts them in a regulatory gray zone – where standards are evolving, but not yet unified.
We partner only with GMP-certified laboratories, demand full documentation of donor screening, viral testing, and batch consistency – and we operate under a medical license with informed consent, ethical review, and child protection protocols in place.
In simple words:
This is not an experimental free-for-all. Exosome therapy may be new, but it demands old-school discipline: medical judgment, transparency, and respect for the child’s biology.
When done right, it’s a promising tool. When done recklessly, it’s irresponsible.
And that’s a line we never cross.
Who Might Benefit Most – And When
Not every child with autism needs exosome therapy. That may sound unusual coming from someone who offers it – but it’s the truth. This isn’t a universal treatment. It’s a targeted tool, best used when the child’s biology and symptoms match the mechanism of action.
So who are the children we tend to see respond?
1. Children with signs of neuroinflammation
These are often the children whose autism presents with:
- Frequent meltdowns, rage episodes, or self-harm
- Unexplained sleep disturbances
- Cyclical loss and recovery of skills (regression and reappearance)
- Sudden changes in sensory tolerance
2. Children between ages 3 and 11
This is the sweet spot we see most often in clinical practice.
Why? Because the brain is still highly plastic (higher neural plasticity between theses ages). This means, that neurons have the highest capability of making connections with the other neurons in the brain before age 11. Pathways are forming. Speech centers are still open. The immune system is active, but flexible. If the child’s inflammation is reduced or neural signaling is stabilized during this window, the developmental curve can change direction – not always dramatically, but measurably.
That said, we’ve seen meaningful improvements in older children and even teenagers – especially in emotional regulation and focus. But the younger the brain, the more room we have to support its natural growth.
3. Children with immune dysfunction, gut issues, or chronic infections
Autism doesn’t exist in a vacuum. Many children on the spectrum also struggle with:
- Severe food intolerances
- Leaky gut or chronic constipation
- Histamine dysregulation
- Autoimmune tendencies (e.g., eczema, allergies, PANS/PANDAS)
These children often have a dysregulated gut-brain-immune axis. And because exosomes can circulate systemically and modulate immune responses, they may create the conditions for calmer neurology by addressing systemic inflammation first.

When is the best time to begin?
Honestly? When the child is ready, and the family is stable enough to support the changes. That might sound vague, but readiness matters. If the child is in crisis – sleepless, non-eating, aggressive – you may need to stabilize first. But if the child is plateauing, and you sense there’s something locked inside, that’s often when exosomes make the most difference.
In summary: Exosomes don’t work because a child has “autism.”
They work because a child has a treatable biological imbalance beneath the autism.
That’s the nuance. That’s the key.
Outlook: A Bridge Between Cellular Intelligence and Neurological Care
Every once in a while in medicine, we find something that doesn’t fit into our existing categories. Something that isn’t a drug, isn’t a device, and yet quietly reshapes the way we think about healing. Exosomes are one of those things.
They don’t override the brain. They don’t push it in one direction or another. They carry signals – tiny, biological suggestions – offering the body a chance to self-correct. And sometimes, that’s all the nervous system needs. A nudge. A whisper. A shift in tone.
Autism is not a mistake to be fixed. It’s a different operating system. But when that system is clogged with noise – when inflammation, immune confusion, or toxic signaling interfere – then communication becomes difficult. That’s not the child’s fault. And it’s not their identity either. It’s biology in distress. And biology, when supported carefully, can recover surprising clarity.
That’s the promise of exosome therapy. Not a miracle. Not a shortcut. But a new language for intervention – one that speaks in molecules rather than force.
Of course, we must proceed slowly. With data. With ethics. With long-term follow-up and full transparency. No child should ever become a test subject for someone else’s ambition.
But when the science and the story align – when the child’s symptoms reflect a biological pattern we understand – and when the response confirms what we’ve hoped for quietly… then it’s no longer theory. It’s care. Real, gentle, regulated care.
We still have much to learn. But what I can say with full confidence is this:
The future of autism care isn’t just behavioral. It’s biological and relational. It’s about recognizing the nervous system not as broken, but as responsive – if we speak its language.
And in that future, I believe exosomes will have a quiet but powerful voice.
Warm regards,
Erdinc CIVELEK, MD, PhD (C)
Professor of Neurosurgery
PhD Candidate of Immunology and Stem cell
President of Turkish Society of Stem cell and Cellular Therapies
Get your free consultation
- Need guidance and reassurance?
- Talk to a real person from MedClinics!
- Let's find the perfect doctor together.