Diabetes Type 1 & 2 – C-Peptide & HbA1c – Stem Cell Therapy in Istanbul, Turkey

Clinical Insights by Prof. Dr. Erdinç Civelek, MD, PhD (C)
C-Peptide, HbA1c and the Quiet Hope for a Better Life
Living With Diabetes: Between Numbers and Daily Burden
Some stories begin quietly. A child sits in a doctor’s office, confused, listening to words that will change everything: “Your body doesn’t make enough insulin anymore.”
Here is where stem cell therapy for diabetes comes in.
Lisa is now in her early thirties and a mother, but she heard these words from the doctor when she was 15 years old. Since then, a subliminal fear has been her constant companion, often frustrating her at the thought of having to inject insulin for the rest of her life. And she is simply tired of all the effort she has to put in to be able to live a reasonably normal life. She’s far from alone.
When you have diabetes, you try to live with the disease as best you can. This is often more difficult than it looks from the outside. Not only do you have to keep an eye on your blood sugar levels all the time, measure them, inject insulin, watch what you eat, etc…
Just as important are the effects that are not visible or measurable. Even if you follow all the rules and do everything exactly as the doctor said, you sometimes feel exhausted, more than normal, more than other people around you, you feel insecure, and somehow you don’t feel like going through with it for the rest of your life.
Over the years, treatment has improved. But what if, beyond traditional insulin therapy, there was a way to help the body itself regain some balance – not through hype, but through biology?
That’s where stem cell therapy enters the conversation. It’s not a magic solution. But for some, it may become an important part of their therapeutic journey. Stem cell therapy may be a game-changer for some diabetes patients. Especially when two blood markers – C-peptide and HbA1c – offer a small but meaningful green light.
Let’s dive in …
Table of Contents
Two Types of Diabetes, Type 1 and Type 2
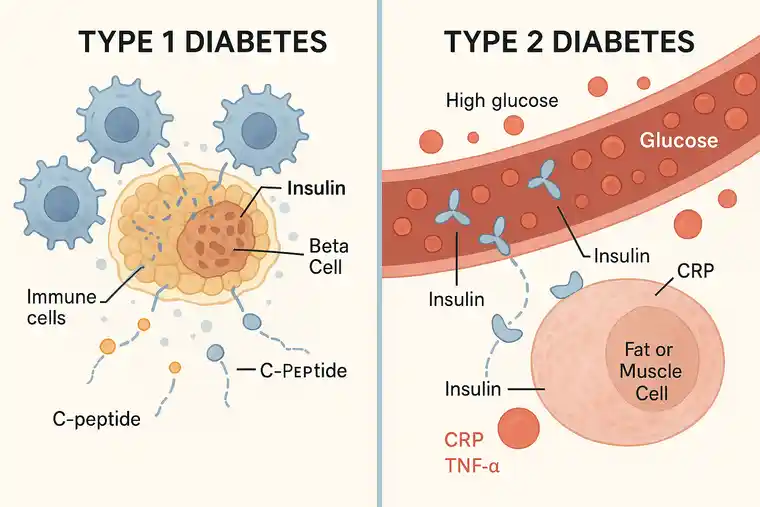
Diabetes Type 1
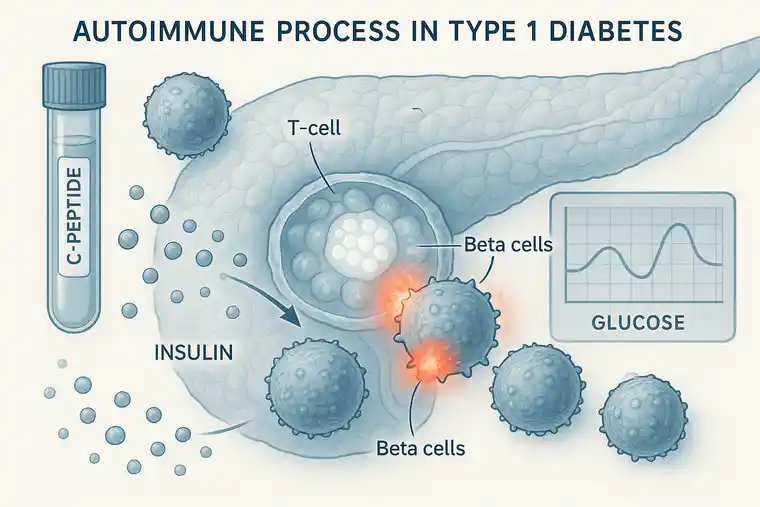
Type 1 diabetes is caused by a misfire in the body’s own immune system. Instead of protecting the pancreas, immune cells begin to attack and destroy the insulin-producing beta cells. Without these cells, the body loses its ability to produce enough insulin — the hormone that keeps blood sugar levels in check. This form of diabetes often develops in childhood or adolescence, and people affected typically require insulin therapy for life. The onset can feel sudden and overwhelming.
That said, not every case follows the same path. Especially in the earlier stages of type 1, some patients still have a measurable level of C-peptide, a marker that tells us the pancreas is still producing small amounts of insulin. That remaining function, even if limited, may offer a chance to preserve or support those cells — which is where stem cell therapy might come into play.
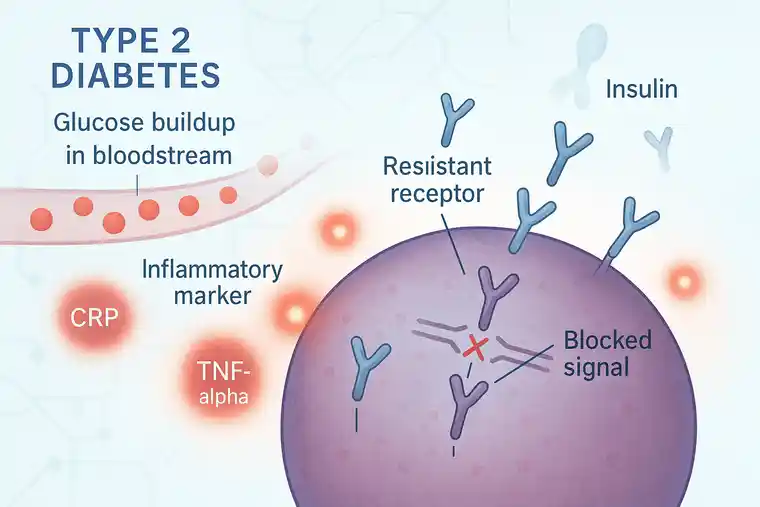
Diabetes Type 2
Type 2 diabetes unfolds more gradually and is rooted in metabolic dysfunction. In these cases, the body either stops responding properly to insulin (insulin resistance) or produces too little of it over time. It’s often linked to lifestyle, chronic inflammation, and genetic predisposition. Many people with type 2 can manage it early on through diet, exercise, or medication, although some may eventually rely on insulin.
To put it simply:
- Type 1 involves an autoimmune attack that shuts down insulin production — though some residual function may still exist at the beginning.
- Type 2 is a slow breakdown in insulin sensitivity and output, shaped by multiple factors.
Knowing the difference isn’t just academic — it’s essential when exploring regenerative options like stem cell therapy, where timing, remaining function, and individual response all play a role.
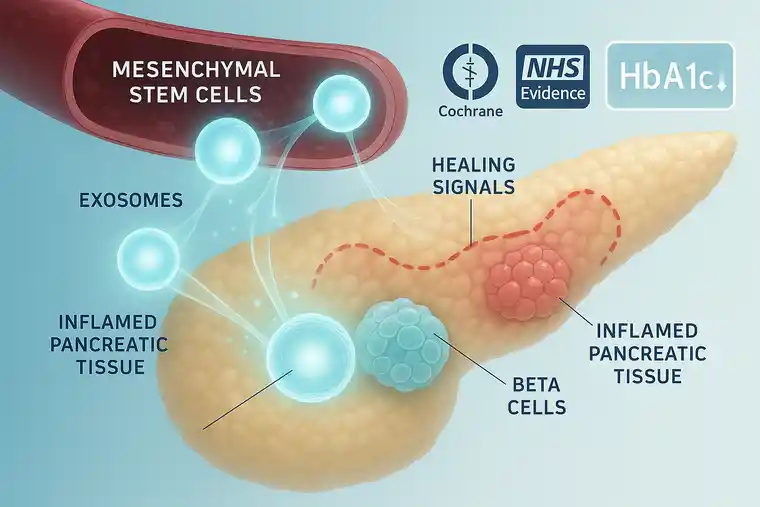
What Stem Cells Do – And Why It Matters for Diabetes
Stem cells are often described as the body’s “raw material” – but they’re much more than that. They are adaptable, intelligent, and responsive to damage. In regenerative medicine, we work primarily with mesenchymal stem cells (MSCs), which can calm inflammation, support cellular repair, and improve signaling between dysfunctional systems.
These cells do not produce insulin themselves. Stem cells prepare the environment for the cells that produce insulin. They reduce inflammation in the body and protect the body from its own harmful immune activities. They help the pancreas and protect it so that it continues to produce insulin, albeit less than normal, and sometimes even manage to restore the pancreas to normal function and ensure that it produces as much insulin as the body needs.
For Type 1 Diabetes:
- MSCs may reduce the immune system’s attack on beta cells. This is immune modulation function of the stem cells which is main goal in treatment of all autoimmune diseases like Type 1 DM.
- They can stabilize inflammation and support tissue recovery in the pancreas.
For Type 2 Diabetes:
- MSCs can improve insulin sensitivity across multiple systems.
- They may help counteract metabolic dysfunction driven by chronic inflammation.
Think of type 1 as an internal civil war – the body attacking its own insulin-producing cells. And type 2 as a communication breakdown – the insulin is there, but the response is broken. MSCs don’t replace the lost cells. But they create a safer, calmer space in which the body might do what medicine alone cannot.
Why We Always Look at These Two Values: C-Peptide and HbA1c
C-Peptide Value
The C-Peptide level in your blood shows if your pancreas is still producing insulin or not. Every time your pancreas makes insulin, it also releases C-peptide in equal amounts. The C-peptide level helps determine whether there’s any remaining beta-cell function. The value should be above 0.2 ng/ml.
If you don’t have enough stem cells in your pancreas, stem cell therapy may not be as effective, because stem cells are not a miracle. They don’t produce insulin themselves, but they inspire your body’s own cells to function better.
HbA1c Value
HbA1c stands for glycosylated hemoglobin. When glucose circulates in your blood, a portion binds naturally to hemoglobin. The HbA1c test shows how much sugar has attached to your red blood cells over time. Since these cells live about 8–12 weeks, the HbA1c test reflects your average blood sugar over the past 3 months – unlike daily finger-prick tests that only show the moment.
In healthy individuals, HbA1c is usually below 5.7%. Between 5.7 and 6.4%, we speak of prediabetes. A value of 6.5% or higher confirms diabetes. For most patients, the target is around 7%, while levels over 8.5% indicate poor control and a higher risk of complications.
In the context of stem cell therapy, a falling HbA1c often points to improved insulin response, reduced inflammation, and a more stable metabolic state – making it one of the most meaningful markers for treatment success.
Is This Therapy for Me? Understanding Suitability
Not every patient is a candidate — and honesty is key.
✅ Type 1 Candidates:
- Detectable C-peptide (typically > 0.2 ng/ml)
- Stem cell treatment also works in some complications of DM, like diabetic neuropathy, nephropathy and retinopathy etc.
- Willingness to follow through with medical instructions
- Stable general health
✅ Type 2 Candidates:
- Patients whose HbA1c level is consistently above 8.5%
- Patients who need to inject insulin or those who suffer from severe insulin resistance
- Patients with systemic inflammation in their bodies. This can be measured using CRP and TNF-alpha levels, among other things.
- Patients who have metabolic problems due to their diabetes. This can manifest itself in excessive weight, persistent fatigue, or fatty liver, among other things.
❌ Unsuitable candidates are:
- People who suffer from type 1 diabetes and whose pancreas no longer produces any insulin. This is measured using the so-called C-peptide value.
- Patients who are actively suffering from cancer, have a severe infection, or have uncontrollable high blood pressure.
- Patients who expect a miracle cure are also not suitable for this treatment. Unfortunately, there are no miracles, and no one can be cured overnight.
A detailed lab analysis is essential. No therapy decision is made without it.
How the Process Works – Step by Step
Step 1: Initial Evaluation
You begin with a real conversation – not a checklist. Your doctor will explore:
- How your diabetes began and how it’s progressed
- What medications and complications are present
- What your goals are, short and long-term
Then, a full diagnostic panel is performed with special attention to C-peptide and HbA1c index. These results determine whether the therapy is safe, medically meaningful, and individually justifiable.
Step 2: Custom Therapy Plan
If you’re eligible, a treatment protocol is created:
- Type and dose of cells
- Number of sessions (usually 1–3, spaced 2–4 days apart)
- Optional supportive modules: exosomes, NAD+, high-dose vitamin C, microbiome therapy
Exosomes, which are extracellular messengers from stem cells, may be used when targeting nerve inflammation or improving neuro-regulation in diabetic neuropathy. Therefore, in some patients we can prefer to use stem cells with exosomes as hybrid cell-based treatment.
Step 3: Outpatient Infusion
On treatment day:
- You’re welcomed and prepped
- Vital signs are checked
- The infusion takes about 45 minutes
- You rest briefly afterward, then return home the same day
The experience is generally calm, often described by patients as “uneventful but quietly hopeful.”
What Can You Expect – And What Not to Expect
What Stem Cell Therapy Won’t Do:
- It won’t replace insulin in type 1 patients
- It doesn’t cure diabetes pathology
- It isn’t a guarantee
What It May Offer:
- HbA1c often decreases within 3–6 months
- Insulin requirements (especially in type 2) may drop significantly
- Glucose fluctuations become less severe
- Fatty liver markers improve
- Many patients report less fatigue, better clarity, more energy
Emotional and Whole-Body Effects:
- Greater sense of control
- Better sleep
- Motivation to care for one’s health returns
- Reduced anxiety over blood sugar “crashes”
- Healthier skin and gum function
- Stronger immune system
- Quicker recovery from illness
- Some patients with neuropathy report subtle sensory return
None of this is guaranteed. But when improvements appear, they are often quiet, gradual – and deeply meaningful.
What Are the Risks?
Minor and Temporary
- Mild tiredness
- Warmth or pressure at infusion site
- Lightheadedness (rare)
These are usually short-lived and easily managed.
Long-Term
- No Long-Term side effects are known
- No link between purified MSCs and tumor growth
- No genetic modification involved
- Risk only arises with unregulated providers – which we firmly reject
We only work with GMP-certified labs that meet EU standards for cell traceability and sterility.
Cell Source and Ethics: A Crucial Question
Our stem cells come exclusively from umbilical cord tissue, donated after healthy births with full consent. These are not fetal or embryonic cells. They are:
- Allogeneic MSCs, tested and certified
- Free of viral, bacterial, or fungal contamination
- Fully traceable
- Screened for over 14 infectious agents
- Immunophenotyped for low rejection risk
We do not use fat-derived cells from the patient – especially not in type 1. The autoimmunity remains and neutralizes the benefit. We rely on high-quality, externally sourced MSCs for consistent anti-inflammatory signaling.
What Science Tells Us About Stem Cell Therapy for Diabetes
Stem cell therapy for diabetes is under active investigation. The data is growing, and here’s what we know so far:
Of course, research is constantly advancing and medicine is constantly making new progress. Studies have already shown that mesenchymal stem cells (MSCs) can be a real therapeutic option. This is especially true for type 2 diabetes or for people with type 1 diabetes who can still produce some insulin themselves.
Clinical studies have shown that MSCs can help lower HbA1c levels. This reduces the daily insulin requirement. MSCs also help reduce systemic inflammation. Patients with type 2 diabetes often experienced significant improvements within the first few weeks after treatment.
Major health authorities, including the NHS and the Cochrane Collaboration, now classify stem cell therapy as a new and potentially significant option, particularly in the context of chronic inflammation and metabolic disorders. The studies also show that stem cell therapy is safe and well tolerated by patients. There are no serious side effects.
Although long-term studies are still lacking, stem cell therapy is very promising, especially in cases where conventional treatments do not help.
Final Thoughts: No Miracle, Just Medicine – and a Human Path Forward
Stem cell therapy is not for everyone. But for those who qualify, it may offer a second line of defense. Not as a replacement for insulin or medical supervision, but as a biological support system – helping the body restore balance in ways medication alone may not.
Ready to Talk?
Contact us now for a free, no-obligation consultation. There’s no cost, no pressure, and no assumptions.
Schedule your free consultation today.
Let’s look at your numbers, your history, and your options – together.
Because diabetes may shape your life. But it doesn’t have to define your hope.
Warm regards,
Erdinc CIVELEK, MD, PhD (C)
Professor of Neurosurgery
PhD Candidate of Immunology and Stem cell
President of Turkish Society of Stem cell and Cellular Therapies
FAQ’s regarding Stem Cell Therapy for Diabetes Type 1 & 2
Can stem cells actually make a difference in diabetes?
They might — but it depends on the person. In type 1 diabetes, the immune system attacks the insulin-producing cells. If even a few are still working, stem cell therapy might help protect them. In type 2, stem cells could support better insulin response and reduce chronic inflammation. It’s not a miracle cure — but in the right case, it may become a meaningful part of a broader plan to manage diabetes more naturally.
When do improvements usually begin after stem cell and exosome therapy for diabetes?
That’s the question everyone asks — and I wish there were a neat answer. But most people don’t feel a sudden shift. It’s not like a switch flips. What happens more often is… you look back after a few weeks and realize something’s eased up. Maybe your sugar levels aren’t jumping around so much. Maybe you’re sleeping better, or you’re not quite as wiped out in the afternoons. Some patients notice they need a little less insulin. But really, it’s your lab results that speak first. The body tends to whisper before it says anything loud.
Why are doctors always checking C-peptide before stem cell treatment?
Because it tells us something insulin tests can’t. Every time your body makes insulin, it also makes C-peptide — like a shadow. If we still see C-peptide in your blood, it means your pancreas is still trying. That’s good news. It means stem cells might still have something to support. Without it, especially in long-term type 1, the stem cell therapy likely won’t help much.
Is stem cell therapy safe for people with diabetes?
Yes, if done in a proper medical setting. Most people feel fine after treatment — maybe a bit tired or warm for a short time. Serious problems are rare, especially when GMP-certified labs are involved. At MedClinics, we only use cells that meet strict safety rules. There’s no gene editing, no fetal cells, no shortcuts. Just regulated medicine, used carefully.
Can exosomes help with diabetes too — or do you need full stem cells?
Exosomes are tiny messengers released by stem cells, and they’re starting to get attention on their own. Exosome therapy alone may offer benefits – especially for people dealing with inflammation or nerve damage, like in diabetic neuropathy. While they don’t replace stem cells entirely, they can act as powerful carriers of healing signals and may play a role in metabolic regulation. For some patients, they’re even added to the stem cell treatment plan for extra effect.
Get your free consultation
- Need guidance and reassurance?
- Talk to a real person from MedClinics!
- Let's find the perfect doctor together.