Exosomes vs. Stem Cells: Myths, Facts & the Overlooked Synergy
A patient-centered perspective on the real power of regenerative medicine
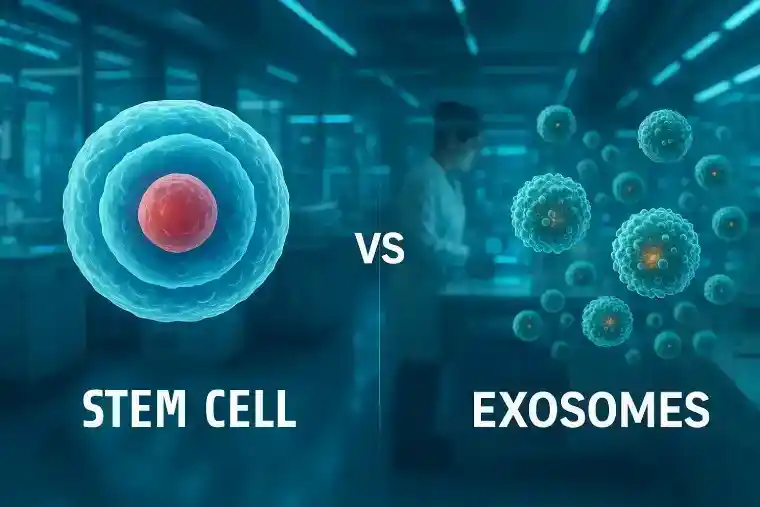
Why Are We Still Comparing Exosomes vs. Stem Cells When We Should Be Combining?
If you follow the latest trends in regenerative medicine, you’ve probably seen the headlines. “Exosomes: the future of cell therapy” or “Stem cells are outdated – exosomes take the lead.” It sounds exciting. Revolutionary. Clean cut. But is it true?
In reality, things are rarely that black and white. As a patient, doctor, or even a curious health enthusiast, it’s easy to get caught in this “either-or” narrative. The truth is, exosomes and stem cells are not rivals. They are partners. Two different languages spoken by the same body. And both are equally vital, depending on the medical need.
In this article, let’s set the record straight. Let’s drop the hype and dig into what science—and experience with patients—truly teaches us.
We will explore:
- What makes exosomes and stem cells fundamentally different—and powerfully complementary.
- Why some common myths still persist.
- And why the smartest approach isn’t to choose, but to combine them wisely.
Table of Contents
Exosomes: The Whispering Messengers of the Body
Imagine a city full of people, buildings, services, and factories. Stem cells are like the construction teams—able to repair, build, and restore. Exosomes? They are the couriers. They deliver instructions, trigger alarms, send repair signals, or call reinforcements.
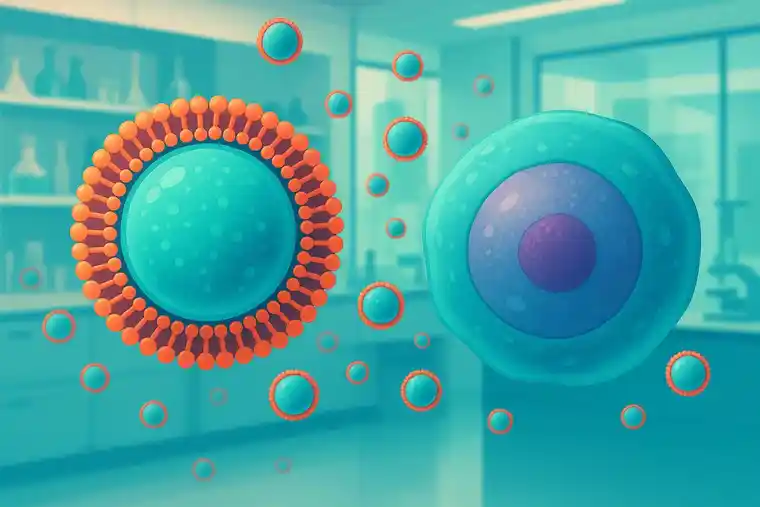
Exosomes are tiny particles released by cells, including stem cells, filled with bioactive “messages.” These messages can include:
- Micro-RNAs, which regulate genes.
- Growth factors that wake up healing cells.
- Proteins and enzymes that calm inflammation or stimulate repair.
But here’s the key difference: Exosomes cannot build new tissues themselves. They instruct, they signal, but they do not act as replacement parts.
This makes them:
- Extremely precise.
- Safer to handle (they can’t multiply or mutate).
- Perfect for calming overreactive immune systems or activating local repair teams.
However, their actions are temporary—they “whisper” to cells but don’t stay around for the heavy lifting.
Stem Cells: The Builders and Architects of Healing

Stem cells, on the other hand, are living repair crews. They are:
- Capable of dividing and creating new, specialized cells.
- Able to integrate into damaged tissues and remain for weeks, months, even years.
They are the body’s most powerful tool for rebuilding what has been broken—be it cartilage in an arthritic knee, skin in a chronic wound, or neurons after a stroke.
But stem cells are not without risks.
- If not carefully sourced or prepared, they can trigger immune reactions.
- In rare cases, they might stimulate unwanted growth.
- And because they are living, they require strict handling, monitoring, and personalization.
Myth 1: Exosomes Are the Better, Safer Alternative
It sounds tempting, right? Why deal with complex, living cells when you can have clean, cell-free exosomes? This is where many headlines mislead.
Reality check:
- Exosomes lack the ability to repair tissue structures themselves.
- They cannot fill in cartilage gaps, replace dead neurons, or rebuild skin layers.
- Their effects fade without the ongoing presence of source cells.
Yes, exosomes are excellent at calming inflammation, stimulating local repair signals, and modulating immune reactions. But they cannot and will not replace stem cells where true rebuilding is needed.
Myth 2: Exosome Therapy Is Risk-Free
This is one of the most dangerous misunderstandings spreading today. Just because exosomes are cell-free and treatment is a cell-free treatment does not make them side-effect-free.
- Poorly sourced, contaminated, or improperly matched exosomes can aggravate autoimmune responses.
- Accelerate unwanted tissue growth (e.g., in fibrotic conditions or near tumors).
- Cause allergic reactions, if not carefully purified.
Also, every exosome “speaks” the language of its source cell. An exosome from a young, healthy mesenchymal stem cell is not the same as one from an aged, stressed skin cell. This is why exosome sourcing, preparation, and quality control must be as rigorous as in stem cell therapies.
Myth 3: Stem Cells Are Yesterday’s Technology
Let’s make this clear: Stem cells are not obsolete. Far from it.
In fields like:
- Orthopedics (e.g., arthritis, tendon injuries).
- Neurology (e.g., stroke recovery, spinal cord injuries).
- Autoimmune modulation (e.g., multiple sclerosis, lupus).
Stem cells continue to be the gold standard when we aim for long-lasting, structural repair and immune resetting.
Moreover, thanks to:
- Allogeneic cell banks.
- Standardized mesenchymal stem cell (MSC) lines with low immune reactivity.
- Combination protocols with exosomes to enhance safety and speed.
Stem cell therapies are safer, more accessible, and more reliable than ever before.
Exosomes enhance them—they do not replace them.
Why Fight When They Can Work Together? The Untapped Synergy
If there’s one lesson clinical studies are now teaching us, it’s this:
Exosomes + stem cells = smarter, faster, safer outcomes.
Why?
- Exosomes act as the “first responders”, calming inflammation, preparing tissues, signaling local cells.
- Stem cells act as the “repair team”, staying behind to rebuild, integrate, and restore.
Examples where this duo shines:
Joint regeneration (e.g., knee osteoarthritis):
Studies show that patients receiving combined exosome-stem cell treatments report faster pain relief, improved mobility, and better cartilage integrity compared to either therapy alone.
Skin and hair rejuvenation:
In aesthetics, the combination leads to faster visible improvements, better skin texture, and more robust hair follicle stimulation—without aggressive procedures.
Autoimmune disorders:
Exosomes calm the storm. Stem cells retrain the immune system for the long haul, it’s not exosomes vs. stem cells, it’s a together.
A Patient-Centered Perspective: Caution, Wisdom, and Realistic Hope
At the heart of all this, let’s not forget what truly matters: patients, not technologies.
Neither exosomes nor stem cells are magical. Both require:
- Personalized protocols.
- Realistic expectations.
- Careful monitoring and evidence-based adjustments.
As a patient, it’s important to ask:
- Is my condition more about inflammation control, immune reset, or structural repair?
- Does my provider understand the difference—and the synergy—between both therapies?
- Am I being offered individualized, ethically sourced treatments—or hyped, one-size-fits-all promises?
Conclusion: The Real Future of Regenerative Medicine Lies in Intelligent Combinations
Let’s move past the false debate and not think about exosomes vs. stem cells. Let’s embrace what science and clinical wisdom are already showing us:
Exosomes and stem cells are two sides of the same coin. Two languages spoken by our healing systems. Two tools that, together, make treatments safer, faster, and more complete.
For the patient of tomorrow, the smartest therapies won’t ask “which one?” They will ask “when and how do we use both?”
And that is where the real innovation lies.
References
- Kalluri, R. (2020). The biology, function, and biomedical applications of exosomes. Science, 367(6478). DOI: 10.1126/science.aau6977
- Phinney, D. G., & Pittenger, M. F. (2017). Concise Review: MSC-Derived Exosomes for Cell-Free Therapy. Stem Cells, 35(4), 851–858. DOI: 10.1002/stem.2575
- Lener, T. et al. (2015). Applying extracellular vesicles based therapeutics in clinical trials – an ISEV position paper. Journal of Extracellular Vesicles, 4(1). DOI: 10.3402/jev.v4.30087
- Cosenza, S., Ruiz, M., Toupet, K.,
by Dr. Deniz Kök
Get your free consultation
- Need guidance and reassurance?
- Talk to a real person from MedClinics!
- Let's find the perfect doctor together.