Spinal Cord Injury – SCI – Stem Cell & Exosome Treatment in Istanbul, Turkey

Understanding Spinal Cord Injury and the Role of Regenerative Therapy for Patients
Clinical Insights by Prof. Dr. Serdar Kabataş, MD, PhD (C)
A Personal Perspective
I’m Prof. Dr. Serdar Kabataş, a neurosurgeon who has spent over twenty years working with patients who have serious central and peripheral nervous system diseases (brain, spinal and peripheral nerve injuries, tumours, aneurysms, etc.). At that time, I’ve seen the limits of what traditional medicine can do – and I’ve also seen how new ideas can push those limits.
In recent years, my focus has shifted toward stem cell treatments and more recently, exosome-based treatment and their potential to help the spinal cord recovery after injury. Spinal Cord Injury is one of the most difficult conditions we face, and one where even small improvements can change the course of a life.
The work in this field is still young, but the possibilities it holds are worth exploring and science is moving forward.
These novel approaches offer hope – not in the form of magic cures, but as tools to help the brain recover in ways we once thought impossible.
Table of Contents
Stem Cell Treatment for Spinal Cord Injury in Istanbul: From First Moments to Hope
If you’ve ever watched a city at night from above – the lights, the moving cars, the endless connections – you’ve seen something a bit like your nervous system. Now imagine one of those main highways suddenly shutting down. That’s what a spinal cord injury feels like. In the space of a heartbeat, the line between brain and body is broken.
People describe the first moments in different ways. Some remember the sound – the crash, the snap. Others remember nothing until they wake up in a hospital bed, confused why their legs won’t move or why their hands feel… strange.
Spinal cord injuries, or SCIs as doctors shorthand them, can come from all sorts of situations – a car accident, a fall, a wrong turn on the sports field, even certain illnesses or circulation problems. But no matter the cause, there’s always that early fog of questions: What exactly happened? Will I walk again? What comes next?
In this guide, I’ll walk you through what we actually mean by “spinal cord injury.” We’ll talk about the different ways they happen, what symptoms to expect, how we treat them with tried-and-true methods, and where newer regenerative options – like stem cells and exosomes – might play a role. And along the way, I’ll share the story of one young man whose case is now published in medical literature, because it shows both the promise and the reality of these newer approaches.
Types of Spinal Cord Injury – Looking at the Cause
Doctors often start by asking how the injury happened, because that shapes everything from prognosis to which treatments we consider first.
Traumatic injuries – sudden and forceful
These are the ones you hear about most:
- Car or motorcycle crashes
- Falls – sometimes from height, sometimes a simple slip in someone whose bones are already fragile
- Contact sports collisions – rugby, American football, ice hockey, diving accidents
- Violence – gunshot or knife wounds to the spine.
The outcome depends on where along the spine the blow lands, how forceful it is, and how quickly the person is immobilized and treated.
Non-traumatic injuries – internal origins
Here there’s no crash, no obvious blow. Instead, something grows, inflames, or compresses the cord from within:
- Tumors, either inside the cord or pressing on it from outside
- Inflammation such as myelitis
- Multiple sclerosis, where the immune system strips away the insulating myelin
- Infections – spinal abscess, tuberculosis
- Degenerative narrowing of the spinal canal, gradually squeezing the nerve tissue.
Ischemic or hypoxic injuries – when blood or oxygen is cut off
These are rarer, but they do happen:
- A blocked spinal artery, a bit like a “stroke” of the spinal cord
- Certain major aortic surgeries, where blood flow to the cord is temporarily reduced
- Severe blood loss or cardiac arrest, depriving the cord of oxygen.
Distinct injury patterns – not all damage is uniform
The cord has different highways for different signals. Damage in certain zones gives recognizable patterns:
- Central cord syndrome – arms weaker than legs
- Brown-Séquard syndrome – one side of the body loses movement and position sense, the other loses pain and temperature sensation
- Anterior cord syndrome – motor function and pain/temperature gone, light touch preserved
- Posterior cord syndrome – the reverse pattern.
Complete vs. incomplete
- Complete: nothing below the injury moves or feels
- Incomplete: some sensation or movement remains – a key factor in potential recovery.
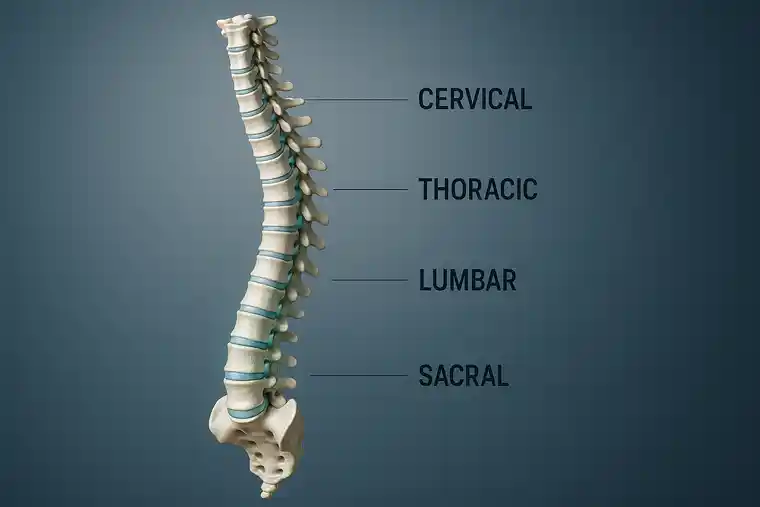
Four Types by Where the Spinal Cord Injury Sits
Now let’s zoom in on location – because an inch higher or lower along the cord can change everything.
Cervical (neck: C1–C7)
When the cord’s injured up high in the neck, all four limbs can be affected – what we call tetraplegia. Above C4, breathing muscles can be involved, and a ventilator may be needed at least initially. Fine hand control is usually impacted, and that makes independence in daily life more challenging. Rehab here isn’t just about strength – it’s about finding clever workarounds for everyday tasks.
Thoracic (upper/mid-back: T1–T12)
These injuries usually mean leg paralysis and less trunk stability, but arms and hands still work. Bladder and bowel control are often an issue. Rehab tends to focus on seated balance, safe transfers, and wheelchair mobility.
Lumbar (lower back: L1–L5)
Here, the legs are the main problem area. The trunk remains stable, so standing and even some walking may be possible with the right aids. Bladder and bowel effects depend on the exact level.
Sacral (pelvic area: S1–S5)
Often partial leg weakness with more prominent bladder, bowel, and sexual function changes. Prognosis for mobility is generally better here than higher up.
Symptoms – What People Notice
What you feel (or don’t feel) after an SCI depends on two things: where the injury is, and whether it’s complete or incomplete.
- Motor: Weakness or paralysis below the level. Fine motor skills, like buttoning a shirt, may vanish
- Sensory: Loss or change in touch, temperature, pain, position sense. Sometimes odd “electric” or tingling feelings
- Secondary: Spasms, chronic pain, pressure sores, breathing changes if the injury is high.
- Autonomic: Trouble with bladder, bowel, blood pressure, sexual function
Many patients ask me this question: I have a spinal cord injury. Can I still have sex?
Of course, a sex life is still part of normal life even after a spinal cord injury. However, things will probably change a little. It often takes some time to figure out how your body works now and what is and isn’t possible.
It is important that you are at peace with yourself and your new normal and that you have a partner who supports you in this.
Causes – with Real-World Faces
- A motorcycle rider flips over the hood of a car, breaking his neck at C5 – complete injury
- A rugby player takes a hit, feels a “pop,” and loses some arm and leg strength – incomplete C6 injury.
- A tumor grows slowly in the thoracic spine; the patient stumbles more over months before surgery removes the pressure.
- A spinal “stroke” leaves both legs weak in minutes.
- A post-viral inflammation turns into sudden paralysis.
- These are different stories, but they all end up under the SCI umbrella.
Conventional Treatment – Step by Step
Acute: Secure the spine, scan, decompress surgically if needed, stabilize blood pressure and breathing. High-dose steroids are sometimes used early, though not in every protocol.
Early rehab: Physical and occupational therapy to protect what’s there, prevent stiffness, and start skill retraining. Breathing therapy if needed. Pain and spasticity management.
Long-term rehab: Wheelchair skills, gait training if possible, adaptive tech, peer support, psychological care. Always tailored – because no two injuries, or patients, are the same.
Stem Cell Therapy – Where It Might Fit for Spinal Cord Injury
If you’ve read about stem cells in the news, you’ve probably noticed two extremes: either they’re painted as a miracle cure or dismissed entirely. The truth, as is often the case in medicine, is somewhere in the middle.
Mesenchymal stem cells (MSCs) – the kind used in the patient case above – are a type of cell that can turn into bone, cartilage, and under certain conditions, even nerve-supporting cells. More importantly for spinal cord injury, they release a soup of helpful molecules – growth factors, anti-inflammatory signals – that can nudge the environment toward healing.
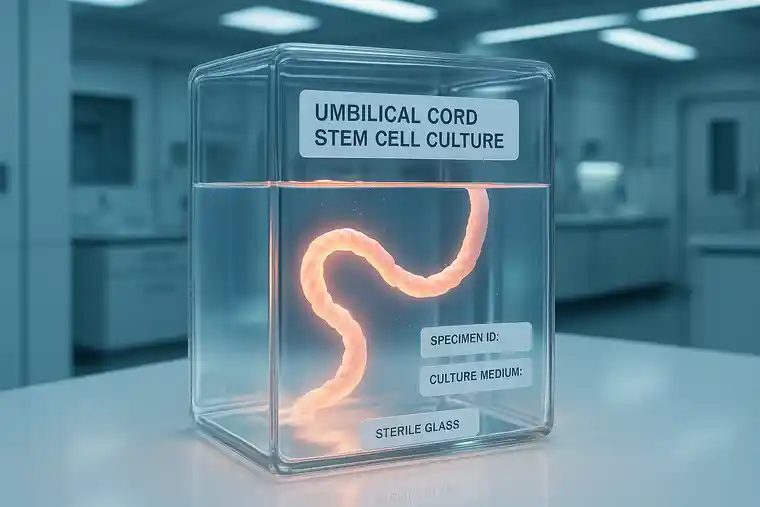
One particular source, Wharton’s Jelly from the umbilical cord, is ethically straightforward. No embryos, no harm to donors. These cells tend to grow well in the lab, and they carry a strong anti-inflammatory profile. In early human use, they’ve shown a good safety track record.
How Stem Cell Treatment for spinal cord injury might help:
- Stem Cells can protect neurons from secondary damage in the early phases
- They reduce inflammation, which is a big player in ongoing damage after the initial injury
- They might help axons (nerve fibers) regrow and re-wrap themselves in myelin
- They can tone down the dense scarring that often blocks regeneration
That said, stem cells are not a solo act. They seem to work best as part of a broader program – surgery if needed, rehab always, and good medical management. The science is still young; many studies are small and uncontrolled. So while the signals are promising, we’re careful not to oversell.

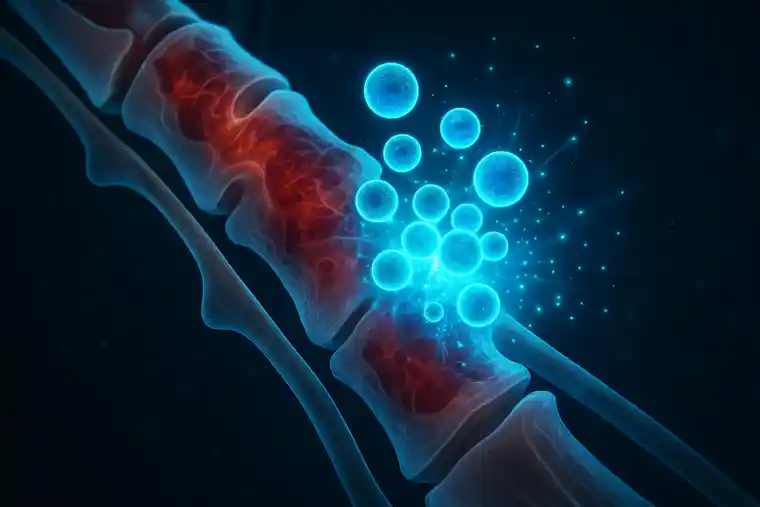
Exosomes – The Tiny Messengers
If stem cells are the factory, exosomes are the packages leaving the loading dock. They’re tiny sacs, thousands of times smaller than a single cell, filled with proteins, RNA, and other messages. When one cell wants to influence another, exosomes are one of the ways it sends instructions.
Why does this matter for spinal cord injury? Because the cord is a hard place to reach. Exosomes can cross barriers that whole cells can’t, including the blood-brain barrier. Once there, they can:
- Dial down inflammation
- Encourage new blood vessel growth
- Support axon regrowth and remyelination.
They don’t divide, so they can’t become tumors. They can be stored and dosed more like a drug. And because they’re cell-free, the risk of immune rejection is low.
Right now, most exosome data in SCI comes from animal studies – but the results have been encouraging. In some models, movement improves, scar tissue is reduced, and nerve tissue looks healthier under the microscope. A few early human uses have been reported, mostly for safety checks, and so far the profile looks good. Still, this is earlier-stage than stem cells, and it needs more robust trials.
What We’ve Seen So Far: Real Stories, Real People
Pepole, who got stem cell treatment for spinal cord injury
A 29-year-old man suffers a complete T6 injury at work. After surgery and months of rehab, no real motor improvement. Then, about 3½ months in, his team adds a regenerative therapy: Wharton’s Jelly-derived mesenchymal stem cells.
Two doses a month for two months. Each dose: 1 × 10⁶ cells per kg body weight. Given into the spinal fluid, into muscle, and into a vein.
He tolerates it well – just mild, brief headaches. Over the next weeks, his lower-limb strength improves, and bladder control gets better. His confidence shifts.
It’s one story, one patient, published in the Journal of Turkish Spinal Surgery. It doesn’t prove stem cells work for everyone – but it shows a possibility worth studying.
Integrating Care – The Real-World Approach
In real clinics, we don’t treat “a spinal cord injury.” We treat this person, with this injury, at this point in recovery.
The strongest results usually come from layering:
- Acute medicine to stabilize and prevent further injury.
- Rehabilitation to push the nervous system to adapt and re-route.
- Regenerative adjuncts like MSCs or exosomes, when appropriate, to change the healing environment.
It’s rarely a matter of choosing one single path and sticking to it. The real progress usually comes when different specialists – the spine surgeon, the rehab doctor, the physio, the psychologist, the urologist, and the nurses – are actually talking with each other, and with you, so everyone’s pulling in the same direction.
Risks and Setting Expectations
No treatment is risk-free. Surgery can bleed or get infected; rehab can cause overuse injuries if it’s not paced right. Even in expert hands, stem cells and exosomes can trigger mild fevers, headaches, or muscle aches for a day or two. Severe problems are rare in regulated settings, but quality control is everything.
Expectations are another part of safety. The gains in stem cell treatment for spinal cord injury, when they happen, are often measured in increments – a bit more strength, fewer spasms, better bladder awareness – not sudden, movie-style recoveries. The wins add up over months, sometimes years, especially with consistent rehab.
One big red flag: anyone promising a cure, dismissing standard care, or refusing to say where their cells come from. That’s when to walk away.
Where the Stem Cells Come From – and Why It Matters
For both, MSCs and exosomes, safety starts long before the treatment reaches the patient.
- Source: Wharton’s Jelly from the umbilical cord, collected after birth with consent.
- Lab work: Processed under Good Manufacturing Practice standards, with sterility checks, potency testing, and verification of cell identity.
- Screening: Donor blood tested for infectious diseases.
- Tracking: Every batch is traceable from donor to recipient.
These steps are why reputable programs can quote good safety numbers. Skip them, and you’re guessing.
What the science says about Stem Cell Treatment for Spinal Cord Injury
Updates on Human Neural Stem Cells: From Generation, Maintenance, and Differentiation to Applications in Spinal Cord Injury Research
https://pubmed.ncbi.nlm.nih.gov/30209662/
This work outlines reliable methods for deriving, expanding, and differentiating human neural stem cells—including those from iPSCs—to ensure they remain multipotent and suitable for research or therapeutic use. It highlights how these well-validated protocols support both laboratory discoveries and early translational efforts in spinal cord injury research.
Multiroute administration of Wharton’s jelly mesenchymal stem cells in chronic complete spinal cord injury: A phase I safety and feasibility study
https://pubmed.ncbi.nlm.nih.gov/40503363/
This phase I trial administered Wharton’s Jelly – derived mesenchymal stem cells via three routes (spinal fluid, muscle, and bloodstream) in patients with chronic, complete spinal cord injury, monitoring them for a year. It reports, that the treatment was safe and associated with meaningful improvements in motor function and quality of life, though results should be interpreted cautiously without a control group.
Before We Finish – A Personal Note regarding Stem Cell Treatment for Spinal Cord Injury
Life after a spinal cord injury isn’t something you adapt to overnight. Your body feels different, your routines shift, and some days will test your patience. But even the smallest wins matter more than people think – being able to sit comfortably through a meal, managing your bladder without stress, standing just long enough to wrap your arms around someone you love.
When we meet a new patient, we don’t start with grand promises. We start with what’s right in front of us: keeping you stable, protecting the function you have, and working with you to build on it. If regenerative options like stem cells or exosomes might help, we bring them into the plan carefully – making sure you know exactly why we think they fit, what the potential is, and where the limits are.
If you, or someone close to you, is living with an SCI, you don’t have to figure it all out on your own. We’re here to hear your story, look over your current care, and talk honestly about what could come next – whether that’s adjusting your rehab, getting another surgical opinion, or seeing if you’re eligible for a well-run research program.
When you’re ready, reach out. No pressure, no scripts – just a real conversation about what matters to you, and how we might help you get there.
Stay updated
Speaking as someone who treats patients and follows the research, I feel we owe it to people to share what we know – without the hype, just plain facts and a clear picture. The story of HIE isn’t finished yet, and there’s a real chance that regenerative medicine could shape what comes next.
About the Author
Prof. Dr. Serdar Kabataş
Neurosurgeon | Stem Cell Researcher & Specialist
Head of Neurosurgery Department | PhD (C) in Stem Cell and Immunology
FAQs about Stem Cell Therapy for Spinal Cord Injury
What exactly is a spinal cord injury – SCI?
A spinal cord injury is always a serious emergency. It interrupts the connection between your brain and your body. As a result, the brain can no longer send signals, or the signals it sends cannot reach your body. This causes sudden limitations in your movement and sensation. It can even affect the functioning of your organs.
What’s the difference between complete and incomplete injuries?
A distinction is made between complete and incomplete injuries.
In the case of a complete injury, the connection is completely severed and no signals from the brain reach the body. This means that you no longer have any sensation below the injured area and cannot move anything below this point.
In the case of an incomplete injury, some signals still reach the area below the injury, so that some movement and sensation below the injured area is still possible.
Which parts of the spine can be affected?
The spinal cord is divided into four regions:
Cervical – neck area, affecting arms, hands, and everything below
Thoracic – upper back, often affecting the chest and legs
Lumbar – lower back, mainly affecting legs, hips, and lower body functions
Sacral – base of the spine, affecting pelvic organs and parts of the legs
Where the damage happens shapes the challenges — and the possibilities — in recovery.
How do these injuries usually happen?
Some patients remember the exact moment — the car crash, the fall, the sharp impact. Others wake up in a hospital bed with only fragments of what happened. Accidents and sports injuries are common, but illness, inflammation, tumours, or even a blood clot can cause similar damage. There’s also a pattern called central cord syndrome, often linked to hyperextension injuries in the neck.
Can stem cells help in spinal cord injury- SCI?
Stem cells aren’t a magic reset button, but for some people they’ve opened a door that had been closed for years. One of our patients — a young man injured in a motorcycle accident — had no movement below his chest for over two years. He was then treated with mesenchymal stem cells from Wharton’s jelly. At the same time, he underwent a rigorous rehabilitation program.
At some point, he noticed small changes, such as a twitch in his thigh that had not been there before. He was also suddenly able to maintain his balance better while sitting.
These may seem like small changes, but for the patient they make a huge difference.
What role might exosomes play?
Exosomes are tiny, natural messengers that cells release to help signal repair. In practical terms, you can think of them as a kind of postal service for healing instructions. We’ve seen cases where exosomes were added to an SCI patient’s program to help calm inflammation and support tissue health, especially in the early recovery phase. They’re still a developing field, but for patients already working hard in rehab, they may act like an extra nudge to the body’s own healing processes — not replacing therapy, but helping it along.
What’s most important after a spinal cord injury?
Time matters. The most important thing is to protect the spine so that further damage can be avoided.
Rehabilitation should then begin as soon as possible, whether through medical care, therapy, or, if possible, stem cell therapy.
Can I still have sex after spinal cord injury?
Of course, a sex life is still part of normal life even after a spinal cord injury. However, things will probably change a little. It often takes some time to figure out how your body works now and what is and isn’t possible.
It is important that you are at peace with yourself and your new normal and that you have a partner who supports you in this.
Get your free consultation
- Need guidance and reassurance?
- Talk to a real person from MedClinics!
- Let's find the perfect doctor together.