Stem Cell Therapy for Autism (ASD) | Trusted Doctor’s Guide & Evidence-Based Care
Stem Cell
How Stem Cell Therapy for Autism can change lifes
Parents rarely forget the moment they first whisper, “Something’s different.” I’ve had parents tell me that, at first, it was just little things. Their child’s eyes would meet theirs, then slide away too quickly. They might wander off to the far corner of the room, choosing quiet over the bustle. Sometimes a sound came from their lips-almost a word-but it stopped halfway, as if it lost its path.
And then there are the stories of bigger moments: a full meltdown in the middle of a supermarket aisle, hands pressed tight over ears when a door slammed, or a bedtime ritual that, if altered, could bring on a flood of tears. If any of this feels familiar, please know you’re not the only one walking this road, and you haven’t missed your moment to help your child. You’re right on time for your child.
In our clinic, I meet families who have tried everything they’re told to try. Speech therapy. Occupational therapy. Behavioral programs. Sensory diets. At first, progress comes—little victories that feel enormous. Then, for many children, things plateau. The question I hear again and again is simple and honest:
“Is there anything that reaches deeper – into the biology – so the therapies we already do can work better?”
There isn’t a miracle switch for autism. But there is a biological pathway we can support. Over the last decade, I’ve worked with families using mesenchymal stem cell (MSC) therapy for autism, often alongside exosome therapy, to calm inflammation, nudge immune balance toward health, and create conditions in which development is more likely to unfold. What follows is a careful, practical guide – what this treatment is, what it is not, and how we walk the road with you.
Table of Contents
Autism Beyond Behavior: What We Don’t Always See
We recognize autism by what we can observe: language delays, limited eye contact, repetitive movements, sensory sensitivities, difficulty with transitions. But behavior is the surface. Underneath, many children on the spectrum show patterns that biology can explain:
- Chronic neuroinflammation. It is often chronic inflammation that disrupts the normal transmission of signals..
- Immune dysregulation. The protective and calming arms of the immune system don’t counterbalance the inflammatory side.
- Oxidative stress. Cells face a persistent energy and antioxidant challenge; mitochondria struggle; neurons function less efficiently.
- Gut–brain axis disruption. If the intestinal mucosa is different and there is inflammation, the body constantly receives stress signals. This makes it much more difficult to learn new things.
What Mesenchymal Stem Cells (MSCs) Actually Do for Autism
Stem cells are intended to support the body; they will not replace anything. We only work with GPM-certified laboratories. All cells are carefully tested before they are used on humans. We never use embryonic stem cells or the patient’s own cells.
So what do they do?
- Calm inflammation. MSCs release anti-inflammatory cytokines and growth factors that help shift the neuroimmune state from “danger” toward “repair.”
- Rebalance immunity. They support regulatory pathways and by this way the over-immune activation slows down.
- Protect neurons. In this way they activate the body’s own repair mechanisms.
- Enhance neuroplasticity. With a lower inflammation, the brain can work better and make new connections. This is exactly what we want.
I often tell parents: MSCs are like skilled conductors. They don’t play the instruments, but they bring the orchestra into tune so music can happen.
Exosomes: Small Messengers, Big Precision in Autism
Exosomes are derived from stem cells. They are 1000 times smaller than stem cells and can penetrate the blood-brain barrier and act directly where they are needed. We administer exosomes mainly through the nose. Via the olfactory nerve, they reach the brain exactly where they are needed.
- Improve cell-to-cell communication in targeted brain regions.
- Help dial down localized inflammation.
- Encourage synaptic health and functional connectivity.
If MSCs improve the soil, exosomes carry the seeds and instructions for what grows next.

Who Tends to Respond Best to Stem Cell Theray for Autism – and Why Timing Matters
We treat a wide age range, but in our experience the most dynamic responses often occur in children aged 3 to 9. This isn’t a hard rule – older children can and do improve – but during those years the brain is especially plastic. New pathways form faster; regulation skills consolidate more easily.
Our clinical recommendation is a series of sessions rather than a one-off. Many families choose three. The effects accumulate – each treatment nudges the system further toward balance. In our practice, we have seen that most children have shown remarkable progress after three sessions. Whether it be improved speech, better ability to navigate their environment, improved sleep quality, or better control of their anger and emotions.
Of course, there are no guarantees with stem cell therapy, just as there are no guarantees anywhere in medicine. But the results we have achieved so far encourage us to continue. Often, small advances can mean a whole new world for the patient and their environment.
Eligibility and Honesty: Who Is (and Isn’t) a Good Candidate for Stem Cell Therapy for Autism
This therapy is not for everyone at every moment. We review:
- Medical history and current therapies. We want synergy, not conflict.
- You should have realistic expectations
- Comorbid conditions. Seizures, metabolic disorders, or autoimmune issues may alter timing and approach.
- Family capacity. Post-treatment follow-through matters—sleep, nutrition, therapy engagement.
We proceed only if we believe the benefit–risk balance makes sense now. Sometimes the right answer is “not yet.” Families appreciate a clear “why,” and we always provide it.
The Patient Journey: A Walk You Don’t Take Alone
Step 1 – Listening
Our first conversation is long on purpose. I want the whole story: your child’s early development, sensory triggers, therapies tried, school environment, sleep, gut symptoms, what lights them up, and what shuts them down. Data matters. So does texture.
Step 2 – Interdisciplinary review
Our team (pediatric neurology, immunology, regenerative medicine) reviews your child’s case. We screen for contraindications, refine goals, and decide on the safest, most appropriate protocol.
Step 3 – Preparation
We walk you through logistics: timing, travel, what to bring, how to prepare your child. Small details reduce stress—familiar toys, predictable routines, a schedule explained in simple terms.
Step 4 – Treatment day
Calm, unhurried, medically precise. Possible routes:
- IV (intravenous) for systemic immune modulation.
- IT (intrathecal) into cerebrospinal fluid—reserved for specific cases, performed under strict neurological precautions.
- IN (intranasal) for targeted delivery of exosomes to the brain.
- IM (intramuscular) in combined protocols when indicated.
Step 5 – Aftercare and follow-up after stem cell therapy for autism
We don’t disappear. Families update us regularly. We ask about sleep, meltdowns, eye contact, language, sensory tolerance, play, school notes. Some changes emerge in weeks; others unfold over 3–6 months. Progress isn’t always linear. Plateaus happen. Then, often, another step forward.
What Families Often Notice First
Patterns vary, but we commonly hear these within 4–8 weeks:
- Eye contact holds longer; shared attention improves.
- New sounds or words appear; some children move from single words to short phrases.
- Meltdowns become less frequent or shorter; recovery is faster.
- Sleep is deeper and more regular.
- Digestion settles: less bloating, more regular stools, fewer food aversions.
Are these small? On paper, perhaps. In a family’s life, they’re huge. A child turning to their name. A hand reaching for yours. A joke that lands. These moments change the air in a home.

Case Snapshots: Three Different Ages, Three Different Arcs -Experiences with Stem Cell Therapy for Autism
Early childhood (4 years).
- Before: no spoken words, avoids eye contact, daily meltdowns tied to sound sensitivity.
- After session 2: first single words; a brief game with a sibling; fewer hands-over-ears episodes.
- After session 3: two-step instructions followed; more spontaneous check-ins with parents.
Middle childhood (7 years).
- Before: good vocabulary but rigid routines; noise triggers shutdown; transitions are crisis points.
- After therapy series: smoother transitions; tolerates new environments with ear protection and brief breaks; participates in group learning without leaving the room.
Adolescent (13 years).
- Before: repetitive speech loops; limited back-and-forth; prefers solitary activities.
- After therapy series: initiates conversations on shared interests; more emotional nuance; joins family outings without negotiation.
- These are typical of what we see: not the same for every child, but meaningfully similar in their direction.
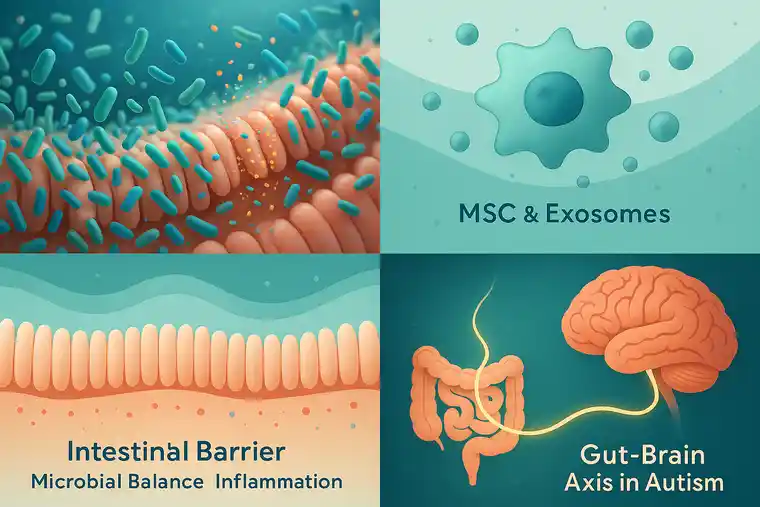
Why the Gut–Brain Axis Matters in Autism More Than People Think
Many children with ASD have gastrointestinal symptoms: constipation or diarrhea, bloating, food sensitivities, pickiness that’s more than preference. We don’t file this under “miscellaneous” – we take everythin seriously regardsing the gut-brain axis.
MSCs and their exosomes support the gut by:
- Strengthening the intestinal barrier, reducing antigen leak that revs up the immune system.
- Promoting a friendlier inflammatory environment, which indirectly supports healthier microbial balance.
- Lowering gut-derived cytokine signals, easing the neuroinflammatory burden on the brain.
Sometimes the gut improves first. Then a month later, language. We’ve learned to watch for that sequence.
How the Stem Cell Therapy for Autism Works
- Cytokine modulation. MSC are able to decrease the molecules, that are responsible for inflammation.
- Microglial recalibration. Brain immune cells shift from a destructive posture to a supportive one, which is friendlier to synapses.
- Synaptic resilience. More connections, better learning
- Oxidative stress relief. Mitochondria perform better; neurons keep up with the energy demands of therapy and daily life.
- Epigenetic nudges. Some exosomal cargo can influence gene expression related to inflammation and plasticity—subtle, not wholesale rewrites.
If all of that sounds technical, the lived effect is simple: a brain that can listen, learn, and connect with less internal noise.
Integration With Ongoing Therapies (This Is Not Either/Or)
We don’t replace your child’s current supports; we unlock them. Families often report that speech therapy “sticks” better, that ABA targets generalize more easily, that occupational therapy sessions feel calmer and more productive. When the body isn’t fighting fires, it has energy for growth. We coordinate with therapists whenever possible so everyone rows in the same direction.
Safety, Ethics, and What to Expect from Stem Cell Therapy for Autism
- Cell source. We use only umbilical cord-derived MSCs from screened donors; no embryonic cells; no autologous cells for ASD (not shown to be effective and may carry dysfunctional immune signals).
- Laboratory standards. Processing occurs in GMP-certified facilities with full pathogen testing and traceability.
- Common short-term effects. Mild fever, fatigue, headache, ore redness at the injection sites. These are expected to disappear within 24-48 hours
What we won’t do. We won’t promise outcomes. We won’t proceed when timing isn’t right. We won’t rush your decision.
Realism matters. Some children improve quickly; others move in waves—progress, plateau, progress. A few show minimal change despite completing three sessions. We talk about all three scenarios in advance. Hope is honest, or it isn’t hope.
What the Science Says about Stem Cell Therapy for Autism
Clinical research on MSCs for ASD is growing. Numerous studies have shown that families reported improvements after treatment, significant improvements in their child’s speech and behavior.
Read for yourself here:
https://pubmed.ncbi.nlm.nih.gov/31097668/
https://pubmed.ncbi.nlm.nih.gov/32033002/
https://pubmed.ncbi.nlm.nih.gov/33535376/
https://pubmed.ncbi.nlm.nih.gov/37905871/
Long-Term Monitoring: What We Track and Why
Change is more than a feeling; it’s a pattern. We encourage families to keep a simple log from day one:
- Sleep: bedtime, night wakings, morning mood.
- Language: new sounds/words, spontaneous use, two-step requests.
- Engagement: eye contact, shared play, initiation of social bids.
- Regulation: meltdown frequency, intensity, recovery time, sensory triggers.
- Gut: stool regularity, bloating, appetite, new tolerated foods.
We also welcome therapist reports and school feedback.
Common Misconceptions (Gently Corrected)
- “This will change who my child is.” No. Our intent is not to erase identity; it’s to remove biological obstacles so your child’s abilities can surface more easily.
- “It’s a one-time fix.” Also no. We see the best results with a series of treatments and continued engagement with therapy.
- “It replaces behavioral or speech work.” It doesn’t. It amplifies it.
- “It’s experimental in the wild-west sense.” Our approach is protocol-driven, ethically sourced, safety-focused, and science-informed.
What parents say after Stem Cell Therapy for Autism
(details have been changed to protect privacy)
- “Three weeks after the second session, he pointed to what he wanted. It sounds small. It was the first time we had a conversation without words.”
- “She still gets overwhelmed in crowds, but she comes back faster. And last week she told a joke. We’ve been waiting seven years to laugh like that together.”
- “School sent an email: ‘Something’s different. He’s participating.’ We cried in the car.”
These aren’t cinematic transformations. They are the kind that matter most—tangible, durable, woven into daily life.
What Makes This Approach Different
Traditional supports work at the behavioral level – and they’re essential. Our work adds a biological first step. By calming neuroinflammation, rebiasing immune tone, and steadying the gut–brain conversation, we make it easier for therapy to “land.” The goal isn’t to force change; it’s to invite it, by making the internal environment more welcoming to learning and connection.
Your Next Step (No Pressure, Just Clarity)
If you’re considering MSC and exosome therapy, here’s how to begin:
- Schedule a consultation. We’ll go through your child’s history and goals in depth.
- Bring every question. Safety, timing, routes, expected timelines—we’ll answer all of it in plain language.
- Decide together.
- Whether you proceed or not, you deserve honest guidance and a team that listens. That part is non-negotiable.
Doctor’s Closing Message
I can’t promise a specific outcome for your child. No one can. What I can promise is integrity – in how we evaluate eligibility, source cells, conduct treatments, and measure change. I can promise partnership – we walk with you before, during, and after therapy. And I can promise attention to the details that make care human: a quieter room, a schedule that respects your child’s rhythm, a phone call returned when you’re worried at 9 p.m.
I’ve learned something from the families who choose this path: progress in autism isn’t a straight line; it’s a series of openings. Our job is to help create the conditions where those openings appear more often – and where you’re ready to walk through them when they do.
FAQ
What are the symptoms of autism?
Autism affects everyone differently, but some common experiences include: struggling with social interactions and talking, engaging in repetitive activities, having narrow interests, feeling overly sensitive to sights, sounds, or textures, being very active or passive, finding change hard, and facing challenges with learning and processing information.
What is stem cell therapy?
Stem cell therapy is a type of treatment that uses stem cells to repair or replace damaged or diseased tissue. Stem cells are undifferentiated cells that have the potential to develop into any type of cell in the body.
How does stem cell therapy for autism work?
Stem cells may be able to help repair or replace damaged neurons in the brain, which could lead to improved social interaction, communication, and behavior.
Contact us now in case you have any questions!
Types of Treatments
Powered by ISSCA, REGEN, and MedClinics - connecting a global network of pioneers to shape the future of regenerative medicine.
Cell-Free Regeneration | The Intelligent Power of Exosomes
Heal from Within | The Power of Stem Cells
Request Form
Get your free consultation
- Need guidance and reassurance?
- Talk to a real person from MedClinics!
- Let's find the perfect doctor together.