HIE – Stem Cell & Exosome Therapy in Istanbul
When the Brain Runs Out of Air: Understanding HIE – Hypoxic-Ischemic Encephalopathy – and the Role of Regenerative Therapy for Patients
HIE (Hypoxic-Ischemic Encephalopathy): Causes, Care & Stem Cells
Clinical Insights by Prof. Dr. Serdar Kabataş, MD, PhD (C)
A Personal Perspective
I’m Prof. Dr. Serdar Kabataş, a neurosurgeon who has spent over twenty years working with patients who have serious central and peripheral nervous system diseases (brain, spinal and peripheral nerve injuries, tumours, aneurysms, etc.). At that time, I’ve seen the limits of what traditional medicine can do – and I’ve also seen how new ideas can push those limits.
In recent years, my focus has shifted toward stem cell treatments and more recently, exosome-based treatment and their potential to help the brain recover after injury. HIE – Hypoxic-Ischemic encephalopathy is one of the most difficult conditions we face, and one where even small improvements can change the course of a life.
The work in this field is still young, but the possibilities it holds are worth exploring and science is moving forward.
These novel approaches offer hope – not in the form of magic cures, but as tools to help the brain recover in ways we once thought impossible.
Table of Contents
Understanding HIE: When the Brain Suffers in Silence
When the Brain Runs Out of Air – A sudden silence in the brain’s city:
Imagine your brain as a vast city. Billions of tiny “lights” – your neurons – send messages down intricate streets, keeping your heart beating, your lungs filling, your arms moving, your thoughts flowing. The city runs 24/7, without pause.
Now imagine that in one sudden moment, the power goes out. Oxygen – the fuel – is cut off. Blood flow – the delivery network – grinds to a halt. At first, some systems manage to run on reserves. But as minutes pass, lights flicker and go dark. When the power finally returns, parts of the city don’t work the same. Some buildings are damaged. Some roads are blocked forever.
This is what happens in hypoxic-ischemic encephalopathy, or HIE. It’s not just an event; it’s a turning point.
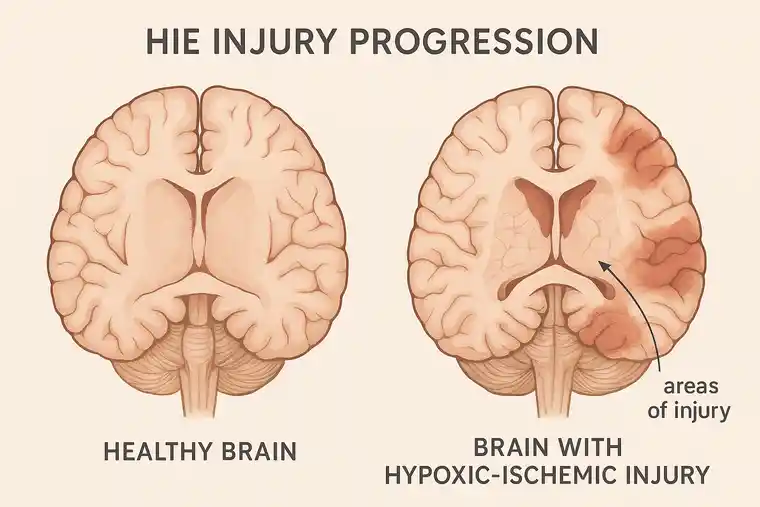
What is HIE, really?
The term breaks down into three parts:
- Hypoxic – not enough oxygen reaching the brain.
- Ischemic – reduced or blocked blood flow to the brain.
- Encephalopathy – a broad term for damage or disease affecting the brain.
HIE is not a single disease. It’s an injury – the result of something else going wrong. In newborns, it can happen during pregnancy or childbirth. In older children or adults, it can follow a cardiac arrest, severe trauma, drowning, or any crisis where the brain is starved of oxygen.
When oxygen and blood flow drop, brain cells begin to malfunction. Some die within minutes. Others enter a stressed state, vulnerable to further damage. The body tries to protect itself, but sometimes these reactions cause more harm: Inflammation surges – the brain’s immune response can destroy healthy tissue along with damaged cells.
The chain reaction inside the brain
- Inflammation surges – the brain’s immune response can destroy healthy tissue along with damaged cells.
- Toxins build up – waste products of struggling cells can poison the environment.
- Blood-brain barrier weakens – harmful substances can leak into areas normally protected.
- Secondary waves of injury – hours or even days later, new damage can occur.
This chain reaction is why speed matters in treatment – but also why recovery is so hard once the initial injury is done.

HIE can strike newborns and adults
Newborns
- Problems with the placenta (too less oxygen delivery before birth)
- Accidents with the umbilical cord
- Very long or very difficult delivery
- Severe maternal bleeding or infection
Children and adults
- Cardiac arrest (sudden stopping of the heart)
- Near drowning
- Choking or suffocation
- Severe head injury
- Major blood loss
- Stroke or blocked blood vessels
Each case is different, but the outcome depends on how long oxygen was missing and how quickly care began.
Life after HIE: what treatment looks like today
Once the immediate crisis is over, treatment moves into two phases
Acute Care
- Restoring oxygen and circulation
- Controlling seizures and swelling
- Cooling therapy (in newborns), which reduces brain temperature to slow damage
Long-term rehabilitation
Recovery here is a routine, not a single procedure.
- Physical therapy to rebuild strength, balance, and coordination
- Occupational therapy for daily tasks like dressing, feeding, and using technology
- Speech and language therapy to improve communication and swallowing
- Medication support keeps symptoms in check – easing spasticity, preventing seizures – so practice actually sticks.
Some patients regain much of their independence. Others remain highly dependent on caregivers. Importantly, none of these therapies repair the damaged brain – they only help patients work around the loss.
The hope for something more: How Stem Cell & Exosome Therapy can help with HIE
Stem Cell Therapy for HIE
For decades, scientists have been fascinated by stem cells – the body’s master builders. They can develop into many different types of cells and release powerful biochemical signals that guide repair.
In brain injury like HIE, stem cells might:
- Calm inflammation, reducing further damage
- Protect neurons that are damaged but still alive
- Promote blood vessel growth to nourish struggling tissue
- Release growth factors that help brain cells reconnect
The goal of stem cell therapy isn’t to “replace” lost neurons. Rather, it’s to support the brain’s natural healing mechanisms – to create the right conditions for neuroplasticity and functional recovery.
Why Wharton’s jelly stem cells are special
A particularly valuable source of stem cells is Wharton’s jelly – the soft, cushioning tissue found inside the umbilical cord. This material contains a high concentration of mesenchymal stem cells (MSCs), which offer several important advantages:
- Collected ethically – obtained from umbilical cords donated after healthy births
- Free from embryo involvement – sidestepping the ethical concerns
- Naturally low risk of immune rejection
- High activity – they release anti-inflammatory and tissue-repairing factors in abundance.
Can stem cells repair a damaged brain?
This is one of the most common – and most important – questions families ask.
The short answer: Not by replacing lost brain tissue in the way most people imagine.
Right now, stem cells cannot rebuild entire networks of neurons with the exact wiring they had before the injury. The brain is far too complex for a “part swap” approach.
Instead, what they can do – based on current research – is help the brain help itself.
Exosome Therapy for HIE
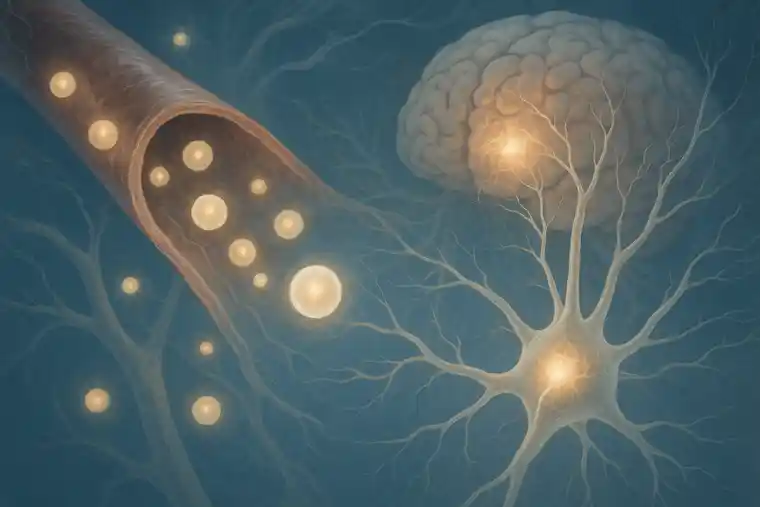
Exosomes are also called the Stem Cells’ Powerful Messengers.
Over time, researchers made an unexpected discovery. It turns out that stem cells might not help the body heal by simply turning into new cells—as many once thought. Instead, much of their power seems to come from how they “communicate” with other cells, sending out tiny messengers known as exosomes.
What are exosomes?
Exosomes are nano-sized vesicles – think of them as microscopic “delivery trucks” loaded with:
- Proteins
- MicroRNAs
- Lipids
- Signaling molecules
These contents can influence other cells — telling them to reduce inflammation, resist injury, grow new blood vessels, or form new synaptic connections.
Why are exosomes so exciting?
- They’re cell-free, which reduces safety concerns like tumor growth
- They can be purified, stored, and standardized
- They can cross the blood-brain barrier
- They can be delivered intravenously, intrathecally (into spinal fluid), or intramuscularly
Exosome therapy is still in its early stages, but it holds the promise of being precise, safe, and scalable.
Where Does Exosome Research Stand?
While human trials are still developing, early animal studies suggest exosomes can:
- Reduce neuroinflammation
- Prevent delayed cell death
- Support tissue regeneration
- Enhance functional recovery
They may soon be tested as a standalone treatment – or in combination with stem cells – to enhance outcomes in patients with brain injury.
What We’ve Seen So Far: Real Stories, Real People
The numbers from early studies give part of the picture, but real lives tell the rest. Have a look at these cases from my studies:
Patient Story: From Heart Failure to Walking Again
A sixteen-year-old boy’s heart stopped, and it took about forty-five minutes of CPR to bring him back. The lack of oxygen left him with serious brain injury — his muscles were stiff, his arms and legs were weak, and he needed a tube in his windpipe to help him breathe.
Four months later, doctors began treatment with stem cells from donated umbilical cord tissue, given in three different ways over several sessions, while he continued intensive rehabilitation. At first, he only felt a touch of fever and some muscle soreness, which soon passed. In the months after, he began surprising everyone – first by sitting up more steadily, then by taking steps with support, and later by managing to dress and feed himself again. By the end of the year, his scans showed no signs of damage, and his strength had almost fully returned.
Read the full study here:
Wharton’s Jelly-Derived Mesenchymal Stem Cell Transplantation in a Patient with Hypoxic-Ischemic Encephalopathy: A Pilot Study
https://pubmed.ncbi.nlm.nih.gov/30203688/
Patient Group Snapshot: Stem Cells in Children with HIE
Six children, all living with serious, long-term effects from hypoxic-ischemic encephalopathy, took part in a pilot treatment program. On average, their brain injuries had occurred nearly two years earlier, caused by prolonged oxygen loss of around forty minutes. Before treatment, they needed help with almost everything – their functional scores were very low, showing severe limits in movement and daily independence.
Doctors used stem cells from donated umbilical cord tissue (Wharton’s jelly), giving them by three different routes over several sessions across two months, alongside continued care and rehabilitation. Apart from short-lived effects like mild fever, headache, or muscle soreness, the treatment caused no problems.
In the months after, small changes began to add up. Some of the children could move more freely, others managed parts of daily life that had been impossible before, and stiffness in their muscles started to ease. By the end of the year, a few were doing things their families hadn’t expected to see again – feeding themselves, taking steps, or playing more actively.
Read the full study here:
Feasibility of allogeneic mesenchymal stem cells in pediatric hypoxic-ischemic encephalopathy: Phase I study
https://pubmed.ncbi.nlm.nih.gov/34136076/
Patient Group Snapshot: Adults with HIE
Eight men and women, most in their thirties, had been living for years with the after-effects of severe brain injury. For many, it began when their heart stopped or they suffered another crisis that cut off oxygen to the brain for nearly three-quarters of an hour. Before the stem cell therapy, they relied heavily on others – walking was difficult or impossible, and daily tasks like dressing or eating on their own were out of reach.
The treatment used stem cells from donated umbilical cord tissue, given in three different ways over the course of two months. Rehab continued alongside. The only side effects were brief and mild – a slight fever, a headache, or sore muscles for a day or so.
Over the following year, the difference was noticeable. Some began to move more freely, others could manage parts of daily life without help, and muscle tightness eased. By the end, a few patients were doing far more for themselves than anyone had expected at the start.
Read the full study here:
Phase I study on the safety and preliminary efficacy of allogeneic mesenchymal stem cells in hypoxic-ischemic encephalopathy
https://pubmed.ncbi.nlm.nih.gov/33821203/
This collection of experiences doesn’t prove that stem cells will work for everyone with HIE – larger, controlled trials are still needed for that. But they do show what’s possible, and they give a human face to what is often just described in numbers and graphs.
What the future might hold
- Stem Cell and Exosome Therapy to be administered early after injury, alongside rehab
- Standardized and stored, ready for emergency use
- Customized to each patient’s age, injury severity, and needs
- Combined with neurostimulation or gene therapy for synergistic effects
But between here and there is a lot of careful science: designing trials, recruiting enough patients, standardizing lab practices, and following participants for years to ensure both safety and lasting benefit.
A grounded kind of hope
HIE is a heavy diagnosis. It changes the path of a person’s life – and often the lives of everyone around them. Right now, recovery is built on therapy, adaptation, and support. Stem cell and exosome research isn’t a magic switch, but it gives us a new tool. Used well, it may help the injured brain recover in ways today’s treatments can’t touch. We should move forward – carefully – with solid trials, strict safety checks, and straight talk about what’s known and what’s not.
The results we’ve seen so far – even the smallest signs of regained function – are enough to justify hope grounded in evidence.
Stay updated
As a clinician and researcher, I believe it’s our responsibility to keep the public informed — not with hype, but with clarity and facts. The story of HIE is still being written, and regenerative medicine may soon play a defining role in the next chapters.
About the Author
Prof. Dr. Serdar Kabataş
Neurosurgeon | Stem Cell Researcher & Specialist
Head of Neurosurgery Department | PhD (C) in Stem Cell and Immunology
FAQ’s rgarding HIE
Can stem cells repair a damaged brain?
This is one of the most common – and most important – questions families ask.
The short answer: Not by replacing lost brain tissue in the way most people imagine.
Right now, stem cells cannot rebuild entire networks of neurons with the exact wiring they had before the injury. The brain is far too complex for a “part swap” approach.
Instead, what they can do – based on current research – is help the brain help itself. Here’s how:
1. Creating a safer environment for recovery
Brain injuries trigger a storm of inflammation. Stem cells can release molecules that calm this storm, making the surrounding tissue less hostile.
2. Protecting neurons on the edge
After HIE, some neurons are damaged but still alive. Stem cells can release protective factors that keep these cells functioning and give them more time to heal.
3. Encouraging rewiring
The brain can sometimes reroute functions to undamaged areas – a process called neuroplasticity. Stem cells can stimulate the growth of new connections to support this.
4. Supporting blood flow
Over time, stem cells can help the body lay down new, delicate blood vessels – the kind you’d never notice, but that quietly carry oxygen and nutrients into places that have been starved since the injury. That extra supply can give struggling brain tissue a better shot at holding on.
It’s nothing like swapping out a broken part in a machine. If anything, it’s more like walking into a tired garden after a harsh season – loosening the earth, shielding what’s still alive, and giving it just enough care for something green to return.
When will we really know if stem cell therapy for HIE worked? And will improvements last?
Some families report small changes like improved flexibility, alertness, or reduced seizure frequency within weeks, but most functional gains appear over several months, often with continued rehabilitation.
How do we know this is legit? What to check before getting stem cell therapy for HIE?
Before making any decisions, there are a few things you’ll want to check – and don’t hesitate to ask directly:
How are the stem cells or exosomes prepared? They should follow strict safety standards — ask if they’re processed under something called GMP. That’s what labs use to make sure everything is clean, consistent, and safe.
Who’s actually doing the procedure? You’ll want to know if the doctors have real experience with brain injuries or regenerative treatments. If it’s a neurosurgeon or a doctor who works in stem cell research, that’s a good sign.
What’s the full plan, start to finish? Try to get a clear picture of the timeline, how many sessions there are, what kind of rehab follows, and whether someone will check in with you after it’s done.
What could go wrong with stem cell therapy for HIE? Is it worth the risk?
So far, treatments appear safe when using ethically sourced Wharton’s jelly (umbilical cord) MSCs or purified exosomes. Some patients report short-lived mild fever, muscle soreness, or headache – but no serious complications . Studies and clinics cite no major adverse effects to date.
Can Stem Cell Therapy & Exosome Therapy really help with HIE?
Let’s be honest – stem cells and exosomes aren’t miracle fixes.
They won’t reverse the damage or rebuild the brain exactly as it was. But what we’ve seen, especially in early-stage studies, is that they may help the brain find new ways to heal. Inflammation seems to calm down, some of the surviving brain cells respond better, and in some cases, we see new connections forming over time.
Some families have noticed things they weren’t sure they’d ever see again – a child sitting more steadily, grasping a spoon, or reacting to voices with more clarity. In a few cases, parents told us their kids started reaching milestones they thought were out of reach.
These changes didn’t happen overnight. It took patience, consistent rehab, and time – but slowly, some movement returned, some independence crept back in.
It’s not a straight path, and not every story is the same, but for some, it’s been a shift in the right direction.
Who can get HIE?
HIE can strike newborns and adults
Newborns
Problems with the placenta (too less oxygen delivery before birth)
Accidents with the umbilical cord
Very long or very difficult delivery
Severe maternal bleeding or infection
Children and adults
Cardiac arrest (sudden stopping of the heart)
Near drowning
Choking or suffocation
Severe head injury
Major blood loss
Stroke or blocked blood vessels
What is HIE?
HIE is not a single disease. It’s an injury – the result of something else going wrong. In newborns, it can happen during pregnancy or childbirth. In older children or adults, it can follow a cardiac arrest, severe trauma, drowning, or any crisis where the brain is starved of oxygen.
When oxygen and blood flow drop, brain cells begin to malfunction. Some die within minutes. Others enter a stressed state, vulnerable to further damage. The body tries to protect itself, but sometimes these reactions cause more harm: Inflammation surges – the brain’s immune response can destroy healthy tissue along with damaged cells.
How can stem cell therapy help with HIE?
For decades, scientists have been fascinated by stem cells – the body’s master builders. They can develop into many different types of cells and release powerful biochemical signals that guide repair.
In brain injury like HIE, stem cells might:
*Calm inflammation, reducing further damage
*Protect neurons that are damaged but still alive
*Promote blood vessel growth to nourish struggling tissue
*Release growth factors that help brain cells reconnect
The goal of stem cell therapy isn’t to “replace” lost neurons. Rather, it’s to support the brain’s natural healing mechanisms – to create the right conditions for neuroplasticity and functional recovery.
Get your free consultation
- Need guidance and reassurance?
- Talk to a real person from MedClinics!
- Let's find the perfect doctor together.