Traumatic Brain Injury – TBI – Stem Cell & Exosome Treatment in Istanbul

Understanding Traumatic Brain Injury and the Role of Stem Cell & Exosome Therapy for Patients
Clinical insights by Prof. Dr. Serdar Kabataş, MD, PhD (C)
A Personal Perspective
I’m Prof. Dr. Serdar Kabataş, a neurosurgeon who has spent over twenty years working with patients suffering from serious central and peripheral nervous system diseases – brain, spinal, and peripheral nerve injuries, tumors, aneurysms, and more. Over those decades, I have seen the remarkable things medicine can achieve, but I have also seen its limits.
In recent years, my focus has shifted toward regenerative approaches – stem cell treatments and, more recently, exosome-based therapies. These methods are not miracles, but they represent a chance to push those limits a little further, especially in conditions like traumatic brain injury (TBI), where even a small gain can change a life.
The work is still young. There are no magic cures. But there are signs that the brain, given the right support, can recover in ways we once thought impossible. And that is why I continue this work.
Table of Contents
What Traumatic Brain Injury Really Means for Patients and Families
When families sit with me after an accident, I often hear the same painful words: “Doctor, he just isn’t the same anymore.”
That sentence captures what traumatic brain injury really means. It is not only the wound on the scalp or the shadow we see on an MRI. It is the sudden transformation of a life.
I have treated young students who went from planning their future careers to struggling with basic speech. I have met fathers who could no longer remember their children’s names, and mothers who grieved not because their child had died but because the person they knew seemed lost inside a living body.
Modern neurosurgery and intensive care save many lives after head trauma. But often recovery slows, progress plateaus, and families ask me: “Is this all we can expect?” For years, my answer was cautious. Today, with stem cell research, I can say: “There may still be a path forward.”
Causes of Traumatic Brain Injury (TBI)
Traumatic brain injury – TBI – arrives without warning. A normal day can turn into a lifetime struggle in a single second.
Road traffic accidents
A violent motion can twist or stretch the brain even without a skull fracture. I recall a 23-year-old who looked unchanged on the outside after a crash, yet his friends told me: “He’s not the same person anymore.”
Falls
Falls are particularly devastating for the elderly. A simple slip in the bathroom can cause bleeding or swelling that permanently changes memory and balance. Children, too, are vulnerable.
Sports injuries
Sports injuries add up quietly. A footballer or boxer may never lose consciousness, but years later shows memory loss and mood changes. I once treated a soccer player whose career ended not with a dramatic knockout, but with the slow accumulation of small blows.
Violence and workplace accidents
Violence and workplace accidents also contribute significantly, leaving young and otherwise healthy people suddenly dependent on others.
No matter the cause, the result is the same: disruption of the brain’s delicate network. Unlike a broken bone, the brain does not heal back to “normal.” The scars may be invisible, but they are profound.
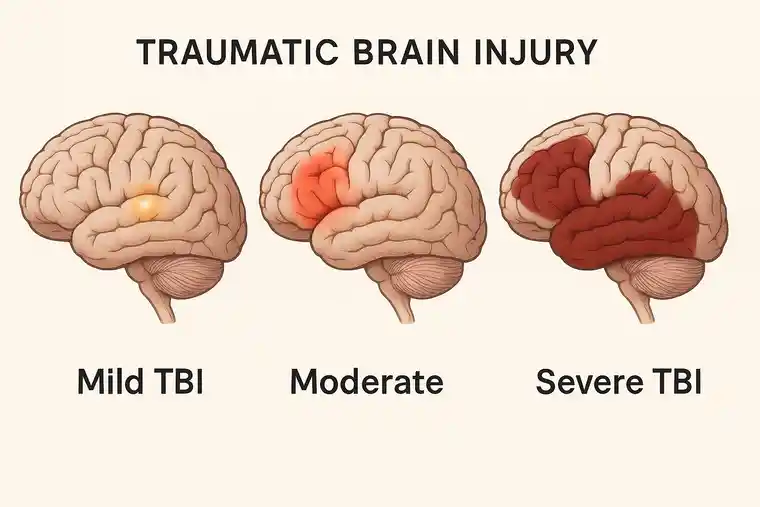
Types of Traumatic Brain Injury and Recovery Differences
Families often ask me: “Why is my son still struggling when another patient with the same accident recovered faster?”
The truth is: no two TBI’s are identical. Outcomes depend on the force, direction, and site of injury – and on the individual brain.
Mild TBI (concussion)
Often underestimated. Patients may look fine, but weeks later complain of fogginess, headaches, and poor concentration.
Moderate TBI
Usually requires hospitalization. Weakness, speech difficulties, and memory problems may persist for months. Some recover well; others do not.
Severe TBI
These are the cases that test us most. Patients may arrive unconscious, sometimes in coma. Even when we save their lives, recovery is uncertain.
Beyond severity, the pattern of damage matters. A bruise on the speech center is different from diffuse microscopic injury spread throughout the brain. This complexity is why families must never compare recoveries.
Symptoms of Traumatic Brain Injury – The Hidden Burden
The greatest challenge with TBI is that many wounds are invisible. A patient may look fine but silently battles deficits every day.
Cognitive changes
Memory lapses, poor concentration, impulsivity. One engineer told me: “I used to design systems. Now I can’t remember my shopping list.”
Physical symptoms
Headaches, dizziness, weakness or seizures. The patient may even feel unsteady when walking across a room.
Sensory loss
Blurred vision, ringing in the ears or loss of sense of taste and smell. I once treated a chef. For him, losing his sense of taste was a disaster.Emotional changes and changes in behavior
Emotional changes and changes in behavior
Irritability, depression or changes in personality. Relatives often miss the person they used to have in front of them; it is no longer the same person.
Sometimes these symptoms can slowly fade or subside, but in other cases they remain permanent. As the symptoms are often not clearly visible are often not clearly visible, think Family and friends think that the person affected well well. In reality, however, patients suffer in silence lacking they often the opportunity to explain themselves because outside everything looks normal from the outside.
Recognizing this reality of traumatic brain injury is essential for both families and society.
Stem Cell Therapy for Traumatic Brain Injury – Clinical Evidence
When I speak about stem cell or exosome therapy, I never promise miracles. What I share instead are the facts – cases and trials that show both safety and potential.
A pilot case (2020)
We treated a 29-year-old man, one and a half years after a severe car accident. Despite rehabilitation, he had plateaued – slurred speech, poor memory, limited motor skills. Over six months, he received six applications of Wharton’s Jelly-derived mesenchymal stem cells (MSC), delivered intrathecally, intravenously, and intramuscularly.
He experienced no major side effects. His speech improved, his memory sharpened, and his fine motor control returned enough to handle everyday tasks. Imaging confirmed genuine changes. For him, this meant regaining independence. For us, it was evidence of possibility.
Read the full article here: https://pubmed.ncbi.nlm.nih.gov/38948099/
Phase I trial (2024)
We expanded to six young adults, aged 21–27. Each received six doses of WJ-MSCs via the same routes.
- Side effects were mild and temporary (low fever, headache, soreness).
- No serious adverse events occurred in a year of follow-up.
- Improvements were measurable: reduced spasticity, better cognitive and motor scores, higher quality of life.
Read the full article here: https://pubmed.ncbi.nlm.nih.gov/33216342/
One patient regained the ability to write short notes after traumatic brain injury. Another could hold a conversation without losing track. These may sound like small steps, but for the patients and their families, they were life-changing.
The Patient Journey in Stem Cell & Exosome Therapy for TBI
Stem cell therapy is not a single event – it is a journey.
- Evaluation – A full review of history, imaging, and current status. Not all patients qualify.
- Planning – A tailored protocol is designed, including dosage and delivery.
- Cell preparation – Umbilical cord tissue is processed in a GMP-certified lab, tested for sterility and potency.
- Treatment – Stem Cells & Exosomes are given across several sessions, alongside rehabilitation.
- Follow-up – We track improvements. Families often notice subtle changes first: a word remembered, a hand less stiff, a smile that returns.
One family once told me that their daughter, who had struggled to hold a spoon for two years, suddenly fed herself without help after the third session. These quiet victories mean more than statistics ever could.
I often tell families: “Do not expect fireworks. Expect a gradual dawn.”
Risks and Realistic Expectations from Stem Cell & Exosome Treatment for Traumatic Brain Injury
Every treatment carries risks. With stem cell therapy for TBI, the risks we have observed so far are mild – temporary fever, headache, or soreness. No serious complications have appeared in our studies.
Equally important are expectations. This is not a cure. It does not erase the traumatic brain injury. What it can do is restore lost functions partially, improve daily life, and open a door where before there was only a wall.
Some patients notice small changes — more stable mood, clearer speech. Others make bigger strides, regaining independence in daily tasks. Families must be prepared for both possibilities. What matters most is that every improvement, no matter how small, can restore dignity.
The Quality of Stem Cells & Exosomes: Responsibility First
Families rightly ask: “Where do these cells come from?”
The stem cells are derived from Wharton’s Jelly in donated umbilical cords, collected only after healthy births with parental consent. They are processed in a Good Manufacturing Practice (GMP)-certified laboratory, screened for infections, and tested for safety and viability.
As a doctor, I would never recommend a therapy I would not trust for my own family. That is why cell quality and ethical sourcing are non-negotiable.
Exosome Therapy – The Future of Traumatic Brain Injury Treatment
Over the past years, I have spoken often about stem cells. Yet there is another part of this field that interests me deeply: exosomes. They are extremely small vesicles released by almost every cell, far too small to be seen with the naked eye. Inside, they carry fragments of RNA, proteins, and other signaling molecules. In essence, they are not cells themselves, but the messages that cells send to one another.
Why is that important for injuries to the brain or spinal cord? Because the central nervous system is difficult to reach. Stem cells are powerfull, Exosomes, in contrast, are small enough to pass through barriers such as the blood–brain barrier and reach regions that larger cells cannot. Once they arrive, they appear to reduce harmful inflammation, support the growth of new blood vessels to improve circulation, and help damaged nerve fibers repair and reconnect.
There is another advantage: exosomes do not divide. That means they cannot form tumors, and the way they can be purified and stored makes them behave more like a medicine than a transplant. For patients, this could one day mean safer, easier dosing, with fewer risks of immune reaction.
At the moment, most of the evidence comes from experimental models. In animals with spinal cord or brain trauma, exosome therapy has reduced scarring, improved movement, and shown clear changes under the microscope. A handful of early clinical uses in humans have already been carried out to check safety – and so far the profile looks reassuring.
Still, I must be honest: exosome therapy is younger than stem cell therapy. The field is at the beginning of its journey, and large, carefully designed trials are needed before we can make strong promises. But I believe that in the future, stem cells and exosomes will not compete with each other — they will complement each other, each adding a different piece to the repair process.
This dual approach may one day expand the possibilities for recovery even further.
Conclusion – Stem Cell & Exosome Therapy for Traumatic Brain Injury – Hope, Grounded in Science
Traumatic brain injury changes not only the patient but everyone around them. Traditional medicine saves lives and helps recovery, but often leaves patients at a plateau.
Stem cell therapy with Wharton’s Jelly-derived MSCs does not promise miracles. But it offers something precious: another chance. I have seen patients regain words, movements, and dignity once thought lost.
Medicine is about more than survival. It is about restoring the person within the patient. With stem cell therapy, and with the emerging promise of exosomes, we are taking cautious but real steps toward that goal.
Frequently Asked Questions about Traumatic Brain Injury Treatment with Stem Cells and Exosomes
Can stem cells cure a traumatic brain injury?
No – they cannot turn back time or rebuild the brain as it was before. What they may do is help in certain areas: a bit more clarity in speech, better control of movement, sometimes sharper memory. I usually explain to families: the aim is to gain back pieces of daily life, not to expect a full reset.
Is the treatment safe?
In the patients we have treated so far, the side effects were minor – a slight fever, headache, or muscle pain that passed quickly. We have not seen dangerous complications. Still, I never call any treatment “risk-free.” We watch every patient carefully.
How soon might changes appear?
That differs greatly. A few patients noticed small steps forward within weeks, such as remembering a name or walking more steadily. For others, it took months. Recovery does not arrive overnight — it’s more like watching daylight slowly return after a long night.
Do I still need rehabilitation if I have stem cell therapy?
Yes, without question. Stem cells are not a substitute for rehab. They may give the brain a better chance to respond, but physiotherapy, speech therapy, and cognitive training remain the backbone of recovery. I often say: stem cells can open the door, but rehab helps you walk through it.
Who might be considered for treatment?
We usually look at patients who are medically stable – not in the acute crisis stage – but still struggling with lasting problems in memory, speech, or movement despite rehabilitation. Every case is unique. A careful evaluation is always the first step before making a decision.
Get your free consultation
- Need guidance and reassurance?
- Talk to a real person from MedClinics!
- Let's find the perfect doctor together.